The Science, Ethics, and Art of Disclosing a Dementia Diagnosis
How can you communicate the diagnosis in a way that relieves suffering and helps patients and their caregivers prepare for the future?
caregiver_chompoo_AdobeStock

Breaking bad news to patients and those who care for them, a stressful event for clinicians of every specialty, presents special challenges when the bad news is a diagnosis of dementia. One definition of medical bad news is “any information that produces a negative alteration to a person’s expectations about their present or future.”1 A diagnosis of major neurocognitive disorder, or dementia in common language, implies changes that will profoundly alter the present and future for an individual with dementia and their caregivers.
Given the cognitive and emotional consequences of this news, particular attention must be paid both to its initial delivery and subsequent processing. Successful communication about a dementia diagnosis requires a complex conversation that includes both discussion of the diagnosis and planning for the future, and it often must transpire over a series of encounters. Preparation for and implementation of this conversation is widely recognized as one of the most demanding tasks in health care.
Physicians’ approach to the disclosure of bad news has evolved considerably over the past several decades, incorporating contributions from many countries and multiple specialties.2 During the 1950s and the 1960s, a diagnosis of cancer was shared reluctantly—if at all—by many physicians. A survey of 180 hospital physicians in Boston published in 1970 reported that only 25% of respondents “always” informed patients about their malignancy—66% informed their patients “sometimes,” and 9% “never” informed patients of their fatal disease.3
An influential book published in 1992 by oncologist Rob Buckman, MD, How to Break Bad News: A Guide for Health Care Professionals, helped transform the discourse from “whether to tell” to “how to tell.”4 In this book, delivery of bad news was presented as a skill that clinicians could both learn and teach. Buckman’s influential 6-point protocol for delivering difficult news will be discussed later in this article.
As a consequence of several factors, the need for effective disclosure and discussion of medical diagnoses in general—and dementia in particular—has gathered new immediacy in our current decade. First, the explosive increase in electronic access to information has meant that patients and families now arrive with more informed assumptions and questions, including questions about new tests and treatments. In the case of dementia, emerging tests are increasing clinicians’ accuracy in earlier and more specific diagnosis. Treatment options have broadened, and many patients wish to know about clinical trials and newly approved therapies.
Second, the 21st Century Cures Act, signed into law by President Barack Obama in 2016, requires that all health care providers give their patients access to all health information available in their electronic health records (EHRs). The immediate accessibility to patients of the information in their EHRs means that patients may first learn about their diagnosis from the online medical record if it has not previously been discussed with them in person by their clinician. Confusion, misunderstanding, and unwarranted anxiety can result when a diagnosis is learned in this way, making it more important than ever for clinicians to time their diagnostic discussion thoughtfully.
Finally, the updated quality measure set for dementia care recently endorsed by the American Psychiatric Association and the American Academy of Neurology includes an element entitled “disclosure of diagnosis.” This measure is defined as the percentage of patients with a diagnosis of a qualifying dementing disorder or disease who have been told (1) that they have dementia and (2) what disease is believed to be causative. The inclusion of this calculation in the measure set reflects the belief that disclosure is a component of good care and the observation that such disclosure often does not occur.5
Patients Want Information, But Disclosure is Not Risk-Free
In the management of neurocognitive disorders, there is evidence that patients and their families desire accurate diagnostic and prognostic information. Eighty-seven percent of respondents without cognitive impairment in a recent study indicated a desire to know of a dementia diagnosis. Among individuals referred to a memory clinic or diagnosed with dementia, 84% “considered full disclosure of a diagnosis of dementia preferable.”6
Broadly speaking, arguments proposed in favor of disclosure are of 3 types. The medical ethics principle of respect for autonomy creates a duty for clinicians to provide patients with information about their health that is needed in order to make health care decisions and to plan for the future. In this light, failing to disclose a diagnosis as significant as dementia may be seen as unethical. From the standpoint of pragmatics, many additional benefits of disclosure have been suggested (Table 1).
Table 1. Advantages of Disclosure of Dementia Diagnosis to Patients and Caregivers
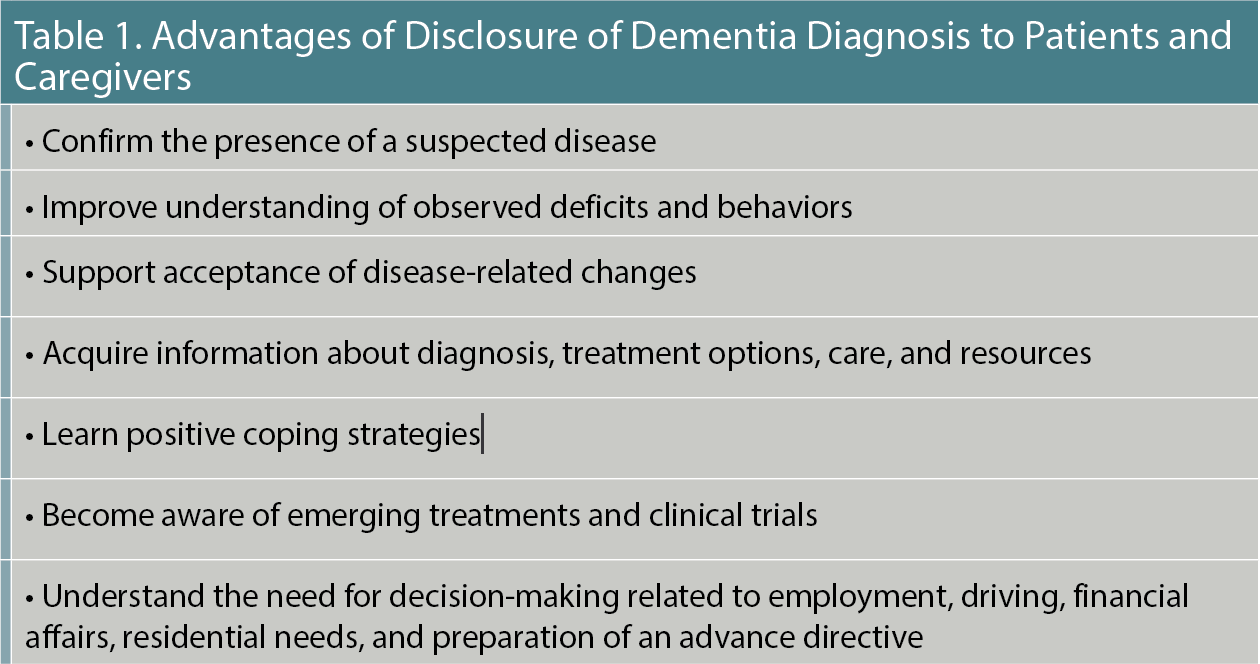
Surveys indicate that patients believe it is important for them to be told the diagnosis so that they can obtain more information, plan, and participate in discussions of therapeutic options. With information and the perspective of a skilled clinician, patients and caregivers are in a better position to engage in shared decision-making.7
Finally, anecdotal evidence supports the idea that disclosure promotes beneficial psychological outcomes. Moore8 noted that “diagnosis (is) an important transition, as it marks a shift from the uncertainty and ambiguity about the early signs and symptoms of dementia to a phase in which the person with the illness and family members can learn to adapt.”
Husband9 reported several cases in which disclosure set the stage for productive psychotherapy leading to relief of anxiety, and to cognitive and behavioral adaptations that improved quality of life. A 66-year-old woman with a strong family history of dementia who presented to him for evaluation of forgetfulness, for example, feared that “health professionals would try to keep information from her and… (that) she would no longer be listened to or involved in decisions relating to her care.” Following the evaluation and the disclosure of her dementia diagnosis, she reported feeling less anxious: “At least I know what it is, I’m not imagining it, and I know what I’m facing.” In her ensuing psychotherapy, “she valued the opportunity to talk about the diagnosis and what it meant to her.” She was able to focus in psychotherapy on “how she could continue to maintain a useful role within her family and social circle, given… her memory dysfunction. This involved negotiating compromises with herself,” which she learned to see as an achievement rather than a failure.
The desire for diagnostic and prognostic information is not independent of expectation, since negative news is more difficult to accommodate. One influential study reported that patients wanted to receive necessary medical information, but also that they were hoping to receive encouraging news.10 Those with serious and advanced disease are often overly optimistic about their own prognosis and less eager to hear bad news.11 Patients’ receptivity to negative news may be affected by how long they expect to live. A study of 214 patients over age 60 with terminal cancer, for example, found that 83% of those who believed they had less than 1 year to live wanted to discuss their prognosis, while only 53% of those who thought they had 2 to 5 years to live wanted to be told their actual prognosis.12 Interestingly, physicians who are in the patient role may illustrate this paradoxical preference to know optimistic news, but avoid discouraging news. In a recent survey, only 72% to 77% of physicians affirmed a wish for disclosure of their own dementia diagnosis; 9% to 13% indicated they would not want to be informed; and the remainder were undecided.6
For patients with progressive impairment of memory and comprehension, the disclosure of a diagnosis can also produce unanticipated consequences. Indeed, concern has been raised by some clinicians and researchers about potential adverse effects of bad news on individuals with dementia and their caregivers. The diagnosis discussion often includes advice that may be difficult to hear about autonomy, driving, and employment. Long-term care insurance or admission to certain long-term residential facilities, for example, may become unavailable. The diagnosis of dementia is associated with considerable public fear and stigma, and it may undermine a patient’s sense of self-esteem and personal value. Feelings of anxiety, depression, increased vulnerability, hopelessness, and burdensomeness can occur. Faced with the possibility of disability, dependence, and progressive decline, some individuals have even become suicidal.
Three studies illustrate the increase in risk of attempted or completed suicide that has been linked with the early phase of dementia. A large analysis of data from adults aged 50 and older derived from cross-linked registers in Denmark showed a relationship between suicide and the presence of a dementia diagnosis. The correlation of suicide with dementia diagnosis was particularly elevated shortly after diagnosis and was threefold higher among adults aged 70 and older. This correlation remained significant when controlled for the presence of mood disorders. The relative risks were even higher among men aged 50 to 69 (RR=8.5) and women aged 50 to 69 (RR=10.8). This study suggested that the initial interval after a dementia diagnosis might usher in a period of increased suicide risk because 26% of the male suicides and 14% of the female suicides occurred within 3 months of dementia diagnosis.13
Another study reviewed findings obtained by linking data from the Georgia Alzheimer’s Disease and Related Dementias registry to data in Georgia’s Vital Records and Violent Death Reporting System. During the study period, 2013 to 2016, 91 individuals with dementia were reported to have died by suicide. In agreement with the observation of Erlangsen and colleagues, one of the identified risk factors identified by Annor and colleagues was a recent diagnosis of dementia.14 Similarly, researchers who studied a large cohort derived from databases associated with the US Department of Veterans Affairs and the Centers for Medicare & Medicaid Services reported on several years of follow-up, which revealed rates for attempted suicide of 0.7% among those with mild cognitive impairment (MCI; 138) and 0.6% of those with dementia (400), compared with only 0.4% of those without MCI or dementia. After adjusting for demographics, medical/psychiatric comorbidities, and earlier diagnosis of MCI or dementia, the suicide attempt risk was found to be highest for those patients with a recent MCI or dementia diagnosis.15
The findings of these 3 studies certainly suggest that the interval following a diagnosis of dementia is a time of increased risk for suicide attempts or completed suicide, but they leave unresolved whether the diagnostic disclosure itself increases or decreases that risk.
Caregivers, typically family members, face additional stresses as a result of disclosure of a dementia diagnosis. Informing family members about the patient’s diagnosis inevitably alters the nature of family relationships. Trust and patient confidentiality may become an issue, especially when the patient wants to take charge of informing, or not informing, family members. With disclosure, family and others may treat the patient in a different way, shifting focus from the individual to their disease and undermining traditional lines of authority and decision-making in the family. The potential for patient abuse or abandonment increases. Family caregivers may also experience more anxiety or depression as they anticipate the burden of what may lie ahead. In addition, some family members may develop fears regarding their own actual or perceived cognitive difficulties or their risk for future decline.
Disclosure Presents Obstacles to Clinicians
According to a recent meta-analysis, only 34.2% of general physicians and 48.3% of specialists usually, regularly, or always told PWDs of their diagnosis.16 Furthermore, disclosure that did occur was often couched in vague, euphemistic terms, using words such as “confusion,” “memory problems,” or “slowing down due to aging” rather than more specific clinical terms such as dementia or Alzheimer disease.16
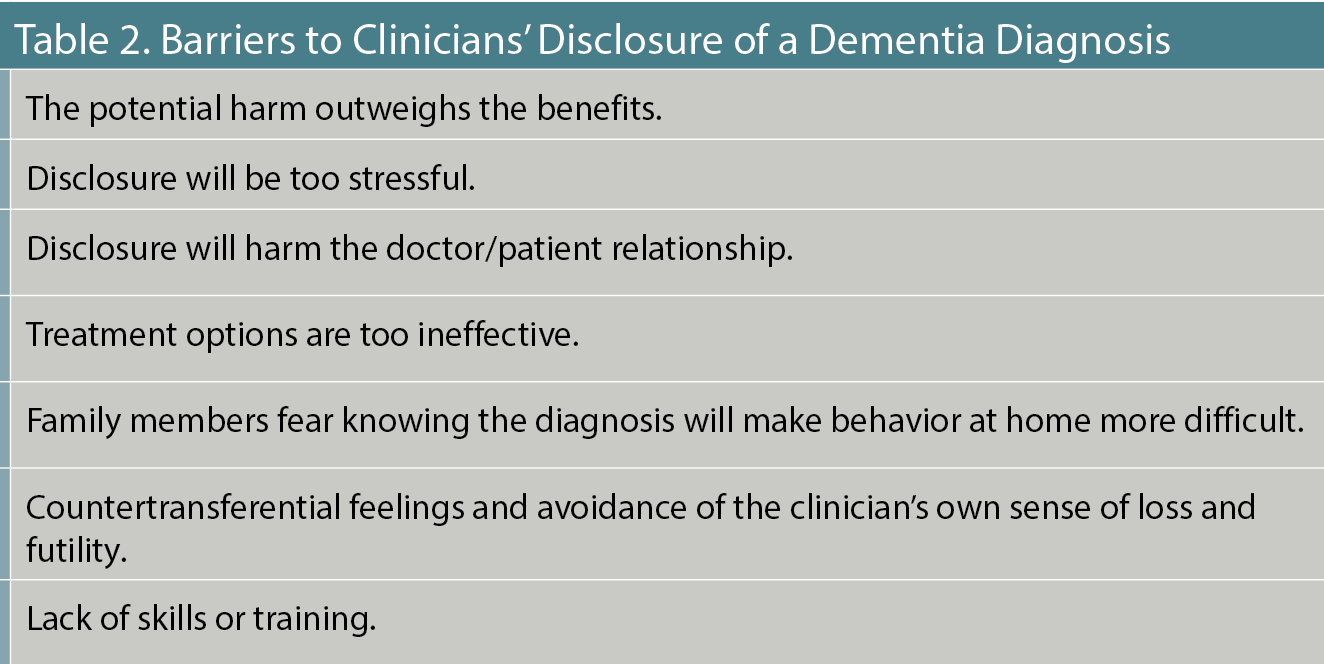
Clinicians are reluctant to break bad news for many reasons. Some invoke “therapeutic privilege” out of concern that risks of disclosure outweigh its benefits. Others may defer disclosure to avoid burdening a patient with bad news.17-23 Clinicians sometimes defer discussion of a diagnosis that may be stressful, stigmatizing, or destructive to the doctor/patient relationship. The fear that treatment options are of limited value may discourage disclosure. At times, family members have urged the clinician to withhold a fearsome diagnosis from the patient out of concern that disclosure will increase the difficulty of care at home.
Clinicians, too, may have difficulty handling their own discomfort and sense of hopelessness about a dementia diagnosis. They may explain their avoidance of disclosure on the basis of diagnostic uncertainty. A study of 343 physicians practicing in outpatient hospice settings found that physicians tended to be inaccurate in their prognoses, and that prognostic errors were more likely to be overly optimistic than overly negative. In addition, prognostic errors tended to increase with increased duration of the doctor/patient relationship.24
Frequently, the reason for the reluctance is the lack of training about how best to disclose a difficult diagnosis, but appropriate clinician training can dispel clinicians’ reservations and improve their disclosure skills. A Cochrane review and meta-analysis of randomized controlled trials and controlled before-and-after trials showed that communication skills training could increase the use of open-ended questions and improve empathy in oncology clinicians.8 More recently, a meta-analysis of 17 studies demonstrated that communication skills training improves physician proficiency and confidence in delivering difficult news.25 Table 2 summarizes important barriers to clinicians’ disclosure of a dementia diagnosis.
Table 2. Barriers to Clinicians' Disclosure of a Dementia Diagnosis
How to Disclose the Diagnosis of Dementia
The actual disclosure process and discussion of a dementia diagnosis can be very stressful events for everyone involved: the patient, the caregivers, and the health care providers. To increase the likelihood of a positive outcome, the clinician can prepare for the clinical encounter by recognizing that disclosure is a process rather than an event, by examining the barriers to disclosure, and by providing information and resources in a way that considers the needs and preferences of the patient and care system.
Even cognitively intact individuals misunderstand or forget much of the clinical information conveyed during a medical discussion. During a disclosure process, caregivers may be personally overwhelmed or distracted by the patient’s discomfort or anxiety. The patient is at an even greater disadvantage in terms of comprehension and knowledge retention. Without appropriate accommodations, they may fail to recall the results, analysis, and suggestions shared by the clinician. It is easy for the patient and caregivers to leave a disclosure discussion with confused or incorrect information.
Absorption and acceptance of difficult information takes time and a recurrent discussion process that gradually evolves and deepens as additional questions arise, as new symptoms evolve, and as new data become available. The initial discussion, therefore, should be conceptualized as the beginning of a dialogue between patients, caregivers, and the health care system. When the initial discussion takes place in a specialist’s office and the patient will be referred back to primary care for follow-up, it may be necessary to direct further questions to the primary care clinician, with an offer of additional support to the primary care clinician from the evaluating specialist.
Delivering complex and disturbing information effectively requires clinicians to overcome a variety of obstacles.26 Clinicians are understandably reluctant to share the bad news of a progressive and usually terminal diagnosis. This is especially the case when the clinician feels the diagnosis is untreatable or that the patient will be unable to make use of the information imparted.27 When the diagnosis of cognitive impairment is uncertain or incomplete, a clinician may delay discussion while awaiting further test results or additional consultations.
Many primary care clinicians and general psychiatrists find themselves in the position of discussing a dementia diagnosis despite limited knowledge of the symptoms, causes, treatment options, and prognosis of the multiple diseases that present with cognitive symptoms. Limited knowledge can create reticence about what to say or how to be helpful. In an effort to delay or avoid creating pain for a patient, clinicians may speak in euphemistic terms, talking about “senior moments” or “age-related memory loss” rather than giving a more precise name to symptoms severe enough to warrant a more accurate designation. The brief time allotted to an appointment can discourage a clinician from tackling a conversation that is unlikely to be finished easily or quickly.
Some evidence suggests, too, that clinicians’ likelihood of disclosing a dementia diagnosis can be influenced by racial and ethnic factors. Lin and colleagues, for example, reported that a higher proportion of non-Hispanic Black and Hispanic patients with dementia were unaware of their condition.28 Recognizing hazards such as these will help clinicians avoid engaging in an incomplete or uninformative discussion.
Meeting the patient’s specific needs requires preparation. First, clinicians can assess patients’ and caregivers’ awareness of relevant symptoms, related health concerns, and lifestyle issues. The values and beliefs of patients and caregivers will affect the ensuing discussion. Understanding the preferences of patients who retain the capacity to make meaningful choices allows clinicians to frame or modify a disclosure discussion and tailor the content to the level of detail desired by the patient.
Families and patients very often come to the disclosure appointment with a strong suspicion regarding an explanation for the behaviors and deficits they have observed. Confirming their hunches can be sad and anxiety-provoking, but also, at a certain level, reassuring and validating. A clear diagnosis may allow caregivers to understand and avoid blaming a cognitively impaired individual whose behavior has become inattentive, inconsiderate, bizarre, uncooperative, frustrating, or even aggressive. An additional decision for more capable patients is who to involve and when they should be included in the sharing of information. When the patient with dementia no longer retains capacity to make appropriate choices in this respect, the clinician will begin discussion with the appropriately chosen surrogate decision-maker.
In discussing diagnosis, clinicians can avoid running short on time by making sure an adequate appointment has been allotted. The discussion, too, can be conducted over more than 1 visit29 following the initial disclosure visit, with an additional visit scheduled in the near future. The level of detail disclosed should match the comprehension and language skills of the participants. Understanding of the important information can be verified through using a “teach back” approach. Clinicians can invite questions and note the emotional reactions of patient and caregiver. Printed resources offer the patient and caregiver additional help in understanding, retaining, and digesting the information discussed. Such materials must be appropriate to the patients’ and caregivers’ language, literacy, and comprehension. A follow-up plan and planned future appointments, whether in specialty or primary care, will help patients and caregivers feel supported during the stressful time of adjustment that follows establishment of a serious medical diagnosis.
The disclosure discussion is grounded in shared, objective, and understandable information. Patients’ reported symptoms, results of diagnostic tests, clinicians’ opinions about the cause of symptoms and which cause is most probable, the expected course of the illness, and the treatment options should all be reviewed, with the goal of reaching a consensus about what is known and what is to be expected. Clinicians, and perhaps especially generalists, may focus excessively on diagnosis, while caregivers’ deeper concerns are about how to obtain emotional and practical supports.30 Caregivers often raise questions about important planning issues such as what to do about employment, residential plans, home safety, driving, financial decisions, and end-of-life planning. Discussion of advance planning, including estate decisions, advance directives, and a will, may be appropriate.
A burning question, often, is how long the patient is likely to survive and what symptom progression should be anticipated. One useful tool for survival prediction was developed and made accessible as a web-based application by Haaksma and colleagues.31 The Global Deterioration Scale32 offers an additional schema for discussing the expected symptoms. Keep in mind that the earlier these discussions take place, the more meaningful the patient’s involvement will be in the planning.
One popular framework for the disclosure of difficult news is the SPIKES approach (Table 3).33
Table 3. The SPIKES Approach33
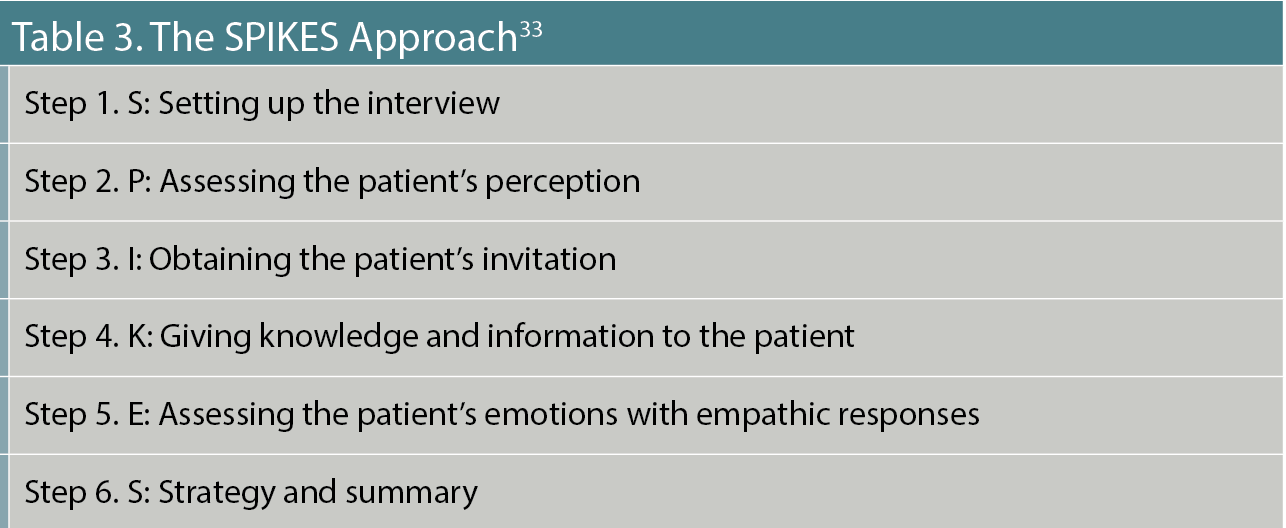
Adaptation of this intervention to discussion of a dementia diagnosis has been described by Peixoto and colleagues,34 who emphasize that setting up the interview for a patient with dementia often requires the presence of a trusted family member because cognitive impairment may limit understanding of the diagnosis discussion. Other companions or clinicians can play helpful roles in the communication as well. Assessing the patient’s perception of this diagnosis requires evaluation of language and comprehension capacity for understanding complex information. When comprehension is sufficiently intact, the discussion should be addressed to the patient. An attempt at obtaining the patient’s invitation is possible even when comprehension is somewhat impaired, and a patient who prefers not to have a diagnostic discussion may wish to delegate this to a caregiver with whom a later communication can be scheduled. Giving knowledge and information to the patient with dementia is a more palatable experience when hope is nurtured by emphasizing some aspects of dementia that are less negative. These include the variable, sometimes slow progression; preservation of personality and capacity for enjoyment in many individuals; availability of palliative treatments; and options for preserving autonomy to the extent possible. Addressing the patient’s emotions with empathic responses includes addressing the emotions of the caregiver, who may be experiencing great distress. And discussion of strategy and summary includes options for rehabilitation and residential choices; legal and safety issues including the stressful, but necessary discussion of driving; and distribution of written information and lists of resources.
The ongoing care of a patient with dementia is a team effort requiring participation of the patient, caregivers, health care providers, and others who will each contribute specialized services. Clinicians can prepare patients and their caregivers for the future by providing lists of helpful books, websites, advocacy organizations, care managers, adult day programs, options for emergency or respite care, and other resources that they may need as the clinical status of the patient evolves.
An important pitfall to avoid with cognitively impaired individuals is that of inappropriate redisclosure. Although a surrogate decision-maker must remain aware of the patient’s deficits, the patient may be unable to understand and retain that information. Repeated questions from the patient about what is wrong, met with a repeated upsetting diagnostic label such as Alzheimer disease may serve to heighten anxiety without beneficial learning. Each new disclosure may be met with shock, fear, or sadness, and these disturbing emotions may linger even after the individual’s cognitive awareness of the cause has faded. It is not necessary or advisable to reexpose an individual to stressful information that cannot be processed and stored. When such questions come up from a patient who has already been informed of the diagnosis, it is preferable to respond with reassurance and redirect the conversation to other topics.
Finally, affirmation of appropriate hope is one of the most valuable contributions clinicians can make. One of the deepest fears the patient will have when diagnosed with a progressive illness is the fear of dependence and possible abandonment. Although the likelihood of a cure cannot be offered at present, the reassuring confirmation of ongoing care and non-abandonment can be provided. There are often means for reducing suffering such as care management, companionship, respite care, symptomatic medications, nonpharmacologic therapies, and exercise. Clinicians can offer some reassurance by emphasizing that much of an individual’s essence remains far into the course of a dementing illness.
With preparation and care, disclosure of dementia diagnosis provides an opportunity for clinicians to educate, relieve suffering, and help patients and caregivers prepare for the future. At present, there is no cure for the common causes of dementia. However, the condition’s increasing prevalence, the growing accessibility of medical information, and our patients’ right to know of their diagnosis require that we engage our patients and their caregivers early in this discussion. Doing so can ease a stressful journey and provide essential support.
Dr Roca is a professor of clinical psychiatry and vice chair of clinical business development in the Department of Psychiatry and Behavioral Sciences at The Johns Hopkins University School of Medicine. Dr Lehmann is clinical director of the Division of Geriatric Psychiatry and Neuropsychiatry, and associate professor of psychiatry and behavioral sciences at Johns Hopkins Medicine in Baltimore, Maryland. Dr Kyomen is a clinical assistant professor at Boston University School of Medicine, an adjunct clinical assistant professor at Tufts University School of Medicine, and a part-time lecturer at Harvard Medical School in Boston, Massachusetts. Dr Ellison holds the Swank Foundation Endowed Chair in Memory Care and Geriatrics, Christiana Care Health System, in Wilmington, Delaware, and is a professor of psychiatry and human behavior at Sidney Kimmel Medical College, Thomas Jefferson University, in Philadelphia, Pennsylvania.
References
1. Buckman R. Breaking bad news: why is it still so difficult? Br Med J (Clin Res Ed). 1984;288(6430):1597-1599.
2. Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet. 2004;363(9405):312-319.
3. Friedman HJ. Physician management of dying patients: an exploration. Psychiatry Med. 1970;1(4):295-305.
4. Buckman R. How to Break Bad News: A Guide for Health Care Professionals. Johns Hopkins University Press; 1992.
5. Schultz SK, Llorente MD, Sanders AE, et al. Quality improvement in dementia care: dementia management quality measurement set 2018 implementation update. Am J Psychiatry. 2020;177(2):175-181.
6. van den Dungen P, van Kuijk L, van Marwijk H, et al. Preferences regarding disclosure of a diagnosis of dementia: a systematic review. Int Psychogeriatr. 2014;26(10):1603-1618.
7. Mariani E, Vernooij-Dassen M, Koopmans R, et al. Shared decision-making in dementia care planning: barriers and facilitators in two European countries. Aging Ment Health. 2017;21(1):31-39.
8. Moore PM, Rivera S, Bravo-Soto GA, et al. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev. 2018;7(7):CD003751.
9. Husband HJ. The psychological consequences of learning a diagnosis of dementia: three case examples. Aging Ment Health. 1999;3(2):179-183.
10. Kutner JS, Steiner JF, Corbett KK, et al. Information needs in terminal illness. Soc Sci Med. 1999;48(10):1341-1352.
11. Lee SJ, Fairclough D, Antin JH, Weeks JC. Discrepancies between patient and physician estimates for the success of stem cell transplantation. JAMA. 2001;285(8):1034-1038.
12. Fried TR, Bradley EH, O'Leary J. Prognosis communication in serious illness: perceptions of older patients, caregivers, and clinicians. J Am Geriatr Soc. 2003;51(10):1398-1403.
13. Erlangsen A, Zarit SH, Conwell Y. Hospital-diagnosed dementia and suicide: a longitudinal study using prospective, nationwide register data. Am J Geriatr Psychiatry. 2008;16(3):220-228.
14. Annor FB, Bayakly RA, Morrison RA, et al. Suicide among persons with dementia, Georgia, 2013 to 2016. J Geriatr Psychiatry Neurol. 2019;32(1):31-39.
15. Günak MM, Barnes DE, Yaffe K, et al. Risk of suicide attempt in patients with recent diagnosis of mild cognitive impairment or dementia. JAMA Psychiatry. 2021;78(6):659-666.
16. Low LF, McGrath M, Swaffer K, Brodaty H. Communicating a diagnosis of dementia: a systematic mixed studies review of attitudes and practices of health practitioners. Dementia (London). 2019;18(7-8):2856-2905.
17. Carpenter B, Dave J. Disclosing a dementia diagnosis: a review of opinion and practice, and a proposed research agenda. Gerontologist. 2004;44(2):149-158.
18. Werner P, Karnieli-Miller O, Eidelman S. Current knowledge and future directions about the disclosure of dementia: a systematic review of the first decade of the 21st century. Alzheimers Dement. 2013;9(2):e74-e88.
19. Milby E, Murphy G, Winthrop A. Diagnosis disclosure in dementia: understanding the experiences of clinicians and patients who have recently given or received a diagnosis. Dementia (London). 2017;16(5):611-628.
20. Mahieux F, Herr M, Ankri J. What are the preferences of patients attending a memory clinic for disclosure of Alzheimer's disease? Rev Neurol (Paris). 2018;174(7-8):564-570.
21. Poyser CA, Tickle A. Exploring the experience of the disclosure of a dementia diagnosis from a clinician, patient and carer perspective: a systematic review and meta-ethnographic synthesis. Aging Ment Health. 2019;23(12):1605-1615.
22. Xanthopoulou P, McCabe R. Subjective experiences of cognitive decline and receiving a diagnosis of dementia: qualitative interviews with people recently diagnosed in memory clinics in the UK. BMJ Open. 2019;9(8):e026071.
23. Lohmeyer JL, Alpinar-Sencan Z, Schicktanz S. Attitudes towards prediction and early diagnosis of late-onset dementia: a comparison of tested persons and family caregivers. Aging Ment Health. 2021;25(5):832-843.
24. Christakis NA, Lamont EB. Extent and determinants of error in doctors' prognoses in terminally ill patients: prospective cohort study. BMJ. 2000;320(7233):469-472.
25. Johnson J, Panagioti M. Interventions to improve the breaking of bad or difficult news by physicians, medical students, and interns/residents: a systematic review and meta-analysis. Acad Med. 2018;93(9):1400-1412.
26. Aminzadeh F, Molnar FJ, Dalziel WB, Ayotte D. A review of barriers and enablers to diagnosis and management of persons with dementia in primary care. Can Geriatr J. 2012;15(3):85-94.
27. Bradford A, Kunik ME, Schulz P, et al. Missed and delayed diagnosis of dementia in primary care: prevalence and contributing factors. Alzheimer Dis Assoc Disord. 2009;23(4):306-314.
28. Lin PJ, Emerson J, Faul JD, et al. Racial and ethnic differences in knowledge about one’s dementia status. J Am Geriatr Soc. 2020;68(8):1763-1770.
29. Grossberg GT, Christensen DD, Griffith PA, et al. The art of sharing the diagnosis and management of Alzheimer's disease with patients and caregivers: recommendations of an expert consensus panel. Prim Care Companion J Clin Psychiatry. 2010;12(1):PCC.09cs00833.
30. Foley T, Boyle S, Jennings A, Smithson WH. “We’re certainly not in our comfort zone”: a qualitative study of GPs' dementia-care educational needs. BMC Fam Pract. 2017;18(1):66.
31. Haaksma ML, Eriksdotter M, Rizzuto D, et al. Survival time tool to guide care planning in people with dementia. Neurology. 2020;94(5):e538-e548.
32. Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139(9):1136-1139.
33. Baile WF, Buckman R, Lenzi R, et al. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302-311.
34. Peixoto VGMNP, Diniz RVZ, Godeiro CO. SPIKES-D: a proposal to adapt the SPIKES protocol to deliver the diagnosis of dementia. Dement Neuropsychol. 2020;14(4):333-339.
