Abstract
Purpose
The number of averted deaths due to therapeutic advances in oncology and hematology is substantial and increasing. Survival of critically ill cancer patients has also improved during the last 2 decades. However, these data stem predominantly from unadjusted analyses. The aim of this study was to assess the impact of ICU admission year on short-term survival of critically ill cancer patients, with special attention on those with neutropenia.
Methods
Systematic review and meta-analysis of individual data according to the guidelines of meta-analysis of observational studies in epidemiology.
Datasource
Pubmed and Cochrane databases.
Eligibility criteria
Adult studies published in English between May 2005 and May 2015.
Results
Overall, 7354 patients were included among whom 1666 presented with neutropenia at ICU admission. Median ICU admission year was 2007 (IQR 2004–2010; range 1994–2012) and median number of admissions per year was 693 (IQR 450–1007). Overall mortality was 47.7%. ICU admission year was associated with a progressive decrease in hospital mortality (OR per year 0.94; 95% CI 0.93–0.95). After adjustment for confounders, year of ICU admission was independently associated with hospital mortality (OR for hospital mortality per year: 0.96; 95% CI 0.95–0.97). The association was also seen in patients with neutropenia but not in allogeneic stem cell transplant recipients.
Conclusion
After adjustment for patient characteristics, severity of illness and clustering, hospital mortality decreased steadily over time in critically ill oncology and hematology patients except for allogeneic stem cell transplant recipients.
Similar content being viewed by others
After adjustment for confounding factors and clustering effect, mortality of critically ill cancer patients has dramatically decreased over the last two decades. This effect is reported in the general population of critically ill cancer patients, including neutropenic patients, but not seen in allogeneic stem cell transplant recipients, patients without mechanical ventilation, and patients requiring renal replacement therapy. |
Introduction
Cancer is the second most common cause of death in North America and Europe [1, 2]. Cancer patients are at high risk of life-threatening complications. Indeed, ICU admission is often required as a result of infection, treatment toxicity and organ infiltration by the underlying malignancy [3,4,5]. Advances in oncology and hematology have led to improved survival in patients with cancer [6,7,8].
It is crucial to determine whether survival has actually improved over time for cancer patients admitted to the ICU with a life-threatening complication. Indeed, besides enabling hematologists and oncologists to inform patients and relatives correctly, it also helps to manage expectations from critical care management. Reports suggest a significant decline in mortality of critically ill cancer patients admitted to the ICU during the last 2 decades. However, the data are limited to unadjusted comparisons and before/after studies without control for changes in case mix and severity over time and across centres, and without attention to admission policies [9,10,11,12,13,14]. In addition, most studies published to date focussed on specific patient populations, such as patients with myeloma, those requiring mechanical ventilation, or allogeneic stem cell (HSCT) recipients [9, 10, 14, 15]. Trends in survival of unselected patients, including those with neutropenia for whom ICU management was deemed futile until recently, have not been explored.
The aim of this systematic review and meta-analysis was to investigate changes in the survival of critically ill cancer patients over time, after adjustment for confounders.
Methods
This systematic review and meta-analysis of individual data was performed according to the guidelines of meta-analysis of observational studies in epidemiology [16] and registered on the PROSPERO database (CRD42015026347). It was a pre-planned follow-up study of a meta-analysis on aggregated data and a previously published analysis of individual data [17, 18].
Study outcome and definitions
The aim of this meta-analysis of individual data was to determine the impact of the year of ICU admission on the survival of critically ill cancer patients. Our hypothesis was that advances in oncology and hematology still translated into improved survival when patients become critically ill.
Neutropenia was defined as a neutrophil count (or in case of missing data as a white blood cell count) less than 1 × 109/L.
Outcome was defined as hospital mortality or 28-day mortality if the former was unavailable [19]. 28-day mortality was used instead of hospital mortality in 1121 patients (15.2%) [18].
Predefined patient populations of interest were patients with neutropenia (presence or absence), patients with solid tumors (as opposed to those with hematological malignancies), and allogeneic HSCT recipients (presence or absence).
Search strategy and eligibility assessment
First, public databases including PubMed and the Cochrane database were searched using Exploded Medical Subject Headings and the appropriate corresponding keywords: “Neoplasm” OR “Malignancy” OR “Cancer” AND “Intensive Care Unit” OR “ICU”. The search was restricted to publications in English and human studies and the time period was May 2005 to May 2015. Abstracts were carefully checked. We excluded case reports and studies focusing on patients younger than 18 years or non-critically ill patients.
Full text of all remaining citations was downloaded for consolidation, elimination of duplicates, and further analysis. Four investigators (Marie Bouteloup, Sophie Perinel, DM, MD) independently assessed the eligibility of all studies identified in the initial search. Disagreements were resolved by discussion among investigators. Last, studies with explicit redundancies were only included once (after agreement by QG and MD).
We checked that approval from a local or national ethics committee in accordance with local regulation was in place for all studies. We also made sure that for prospective studies, patients or their next of kin had consented to participate or had been informed of the study and had not opposed to data collection and analysis.
Data and quality assessment
Corresponding authors of the publications of interest were contacted and invited to collaborate in this study. Authors who agreed to participate were asked to send a file containing individual data including:
Age, gender, year of admission, underlying malignancy (solid tumor vs. hematological malignancy), history of allogeneic SCT, severity of illness score, need for organ support (invasive mechanical ventilation, vasopressor use, renal replacement therapy), neutropenia during ICU stay, neutropenia duration, use of granulocyte Colony-stimulating factors (G-CSF), follow-up and outcome. Authors who did not respond were contacted a second time before being deemed unresponsive.
To enable study comparison, we transformed the severity of illness scores (APACHE II and APACHE III) into the equivalent SAPS II score, using a previously described methodology [18, 20]. When neither APACHE II score nor APACHE III score was available, the existing severity score was transformed into SAPS II score according to the estimated odds of dying during hospital stay. As regard to uncertain reliability of this variable, this later was not used in the current analysis.
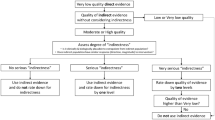
Risk of bias of included studies was assessed using the “risk bias in cohort study” tool developed by the Cochrane group: (http://methods.cochrane.org/sites/methods.cochrane.org.bias/files/public/uploads/Tool%20to%20Assess%20Risk%20of%20Bias%20in%20Cohort%20Studies.pdf; last accessed Feb 02 2017). Results of the search strategy, characteristics of the included studies and risk of bias have been reported in a previous manuscript [18].
Data consistency and completeness were assessed before analysing the rate of missing data, extreme values and data distribution across studies. No imputation was made for missing data. No inconsistency was found.
Statistical analysis
All quantitative variables were described using medians (quartiles) while qualitative variables were described by frequencies (percentage).
Hospital mortality was the variable of primary interest.
Raw change in mortality according to ICU admission year was assessed using Wilcoxon test. Change in mortality over time, weighted for number of observations per year, was plotted for the whole population and for predefined subgroups using mean mortality for each admission year and change over time by linear regression with 95% confidence interval (95% CI).
Independent predictors of mortality were assessed using logistic regression and mixed logistic models. A logistic regression model was built. Variables of interest were selected according to their relevance and statistical significance in univariate analysis. We used conditional stepwise regression with 0.2 as the critical P value for entry into the model, and 0.1 as the P value for removal. The year of ICU admission was planned to be forced in the model in cases where the P value was greater than 0.2. Interactions and correlations between the explanatory variables were carefully checked. Continuous variables for which log-linearity was not confirmed were transformed into categorical variables according to median or IQR. The final models were assessed by calibration, discrimination and relevance. Residuals were plotted, and the distributions inspected. For model building, SAPS II score being correlated with organ supports, underlying tumour, age and neutropenia, these variables were preferred to the SAPS II score and this later was not included in the model.
Then, mixed model was performed using variables previously selected as fixed effect. To investigate both study heterogeneity in the mortality rate and heterogeneity in the effect of the ICU admission year within studies, two random effects were introduced: respectively, a random effect of study on the mean mortality rate (random intercept) and a random effect on the effect of the ICU admission year on within study mortality (random slope) [21]. This model adjusting for clustering effect was planned a priori to be main result of the analysis. Same validation methods were used as previously and calibration was reported as calibration belt [22, 23].
Pre-planned adjusted analyses were performed for the main study population and neutropenic patients.
Last, a post hoc analysis according to use of organ support therapy was performed.
All tests were two-sided, and P values less than 0.05 were considered statistically significant. Analyses were done using R software version 3.4.4 (https://www.r-project.org), including lme4, lmerTest, givitiR packages.
Results
The results of the search are reported in the supplementary appendix. Among the 114 eligible studies, authors of 30 studies (26.3% of selected studies) agreed to participate in this study, resulting in a dataset of 7515 patients, including 1702 neutropenic patients (22.6%) (Figure S1) [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53]. ICU admission year was missing from two studies which were subsequently excluded from the final analysis [36, 44]. Characteristics of the included studies are reported in the supplementary appendix.
Patient characteristics
Among 7356 included patients, mortality data was missing in two patients; both were excluded from the analysis. Of the remaining final cohort (n = 7354), 4889 were included in single center studies (66.5%) and 6029 (82.0%) in 17 prospective studies. Median age was 60 years (IQR 49–69) (Table 1). Overall, 3255 patients (44.3%) had a solid tumour and 438 (5.9%) were allogeneic HSCT recipients. Organ support in the form of invasive mechanical ventilation, vasopressors or renal replacement therapy was required by 3726 patients (50.7%), 3024 patients (41.1%) and 1174 patients (16.0%), respectively. Although studies were published between 2005 and 2015, they reported patients with median ICU admission year of 2007 (IQR 2004–2010; range 1994–2012). Median number of admissions per year was 693 (IQR 450–1007). Unadjusted mortality was 47.4% (n = 3483).
Influence of ICU admission year on mortality
Before adjustment, there was a progressive decrease in hospital mortality throughout the time period (OR per year 0.94; 95% CI 0.93–0.95) (Fig. 1). After adjustment for confounders and adjustment for clustering effect, year of ICU admission remained independently associated with hospital mortality (OR for hospital mortality per year: 0.96; 95% CI 0.95–0.97) (Fig. 2). C-statistic of the mixed model was 0.71 (95% CI 0.70–0.72) and its calibration as assessed by calibration belt is reported in the supplementary appendix shows acceptable curve despite poor goodness of fit (P < 0.001) (Fig. S2).
Predefined subgroups and neutropenic patients
The progressive decline in mortality in the general population was also observed in the subgroups, except in allogeneic HSCT recipients (P < 0.001 for every subgroup except HSTC recipients P = 0.21—Fig. 3).
Change in mortality over time in various predefined subgroup (P < 0.001 for every subgroup except hematopoietic stem cell transplant recipients P = 0.21). Blue line represents linear regression (95% CI) and points represent mean mortality each year and are weighted for number of observation each year
Among the 7354 included patients, 1666 were neutropenic and had full data regarding ICU admission year and outcome available. Their main characteristics are reported in Table S1.
In the neutropenic sub-group, the median age was 55 years (41–64). Two-hundred and eighteen patients (13.1%) had a solid tumour and 186 patients were allogeneic HSCT recipients (11.2%). Invasive mechanical ventilation, vasopressors or renal replacement therapy was required by 939 patients (56.3%), 933 patients (56.0%) and 374 patients (22.9%), respectively. The median ICU admission year was 2008 (IQR 2004–2010; range 1994–2012).
Unadjusted mortality in the studied population was 60.3% (n = 1004). Before adjustment, year of ICU admission was associated with a progressive decrease in hospital mortality (OR per year 0.985; 95% CI 0.98–0.99). Year of ICU admission remained independently associated with hospital mortality after adjustment for clustering effect (OR for hospital mortality per year 0.93; 95% CI 0.91–0.95) (Fig. S3). C-statistic of the mixed model was 0.72 (95% CI 0.70–0.74) and its calibration as assessed by calibration belt is reported in the supplementary appendix shows acceptable curve and goodness of fit (P = 0.26) (Fig. S4).
Post-hoc analysis of patients requiring organ support
Among patients requiring organ support, we explored the influence of ICU admission year on outcome (Fig. 4). Over the 2 decades analyzed, mortality decreased progressively from 100 to 63% in patients requiring mechanical ventilation (P < 0.001) and from 100 to 64% in patients who needed vasopressors (P < 0.0001) but was unchanged over time in patients treated with renal replacement therapy (from 60 to 78%; P = 0.96) (Fig. 4). Similar trend was observed in patients requiring RRT with concomitant need for vasopressors (Fig. S5). Change in organ support being reported in Fig. S6. Influence of ICU admission year remained significantly associated with mortality after adjustment for confounders in all subgroups, except for patients who did not require mechanical ventilation, those who received RRT and allogeneic HSCT recipients (Fig. S7).
Discussion
To the best of our knowledge, this is the first study that confirmed that the outcome of critically ill cancer patients actually improved over the last two decades. After adjusting for main confounding variables and clustering effect, our model suggests that outcomes of patients treated with mechanical ventilation and vasoactive drugs have improved over time. A more recent admission to the ICU was associated with a lower mortality risk in critically ill cancer patients overall, as well as in pre-defined subgroups such as patients with solid tumours, hematological malignancies or neutropenia.
An improvement of the outcome of critically ill cancer patients has been suggested previously by informal comparison across studies [12, 13], in before/after studies [9, 10, 14], and cohort studies including general cancer patients [13], patients requiring mechanical ventilation [12, 13], patients with myeloma [9, 10] or sepsis and HSCT recipients [12, 14, 15]. Apart from a few single-center studies [9, 10], most reports had no or limited adjustment for confounders [12,13,14,15, 54,55,56]. Last, clustering effect, accounting for change in outcome related to unit organization and ICU admission policy were scarcely adjusted for [57, 58].
Our study suggests that survival has improved over time, linearly, after adjustment for confounders. Interestingly, this was observed in the overall population and in various predefined subgroups namely patients with and without neutropenia, patients without HSCT and patients with solid tumours and hematological malignancies.
This study identified a similar pattern of improved outcomes over time in the pre-defined subgroup of neutropenic patients. Despite the relatively high ICU and hospital mortality, patients with neutropenia have progressively benefited from changes in general clinical management when adjusting for usual confounders and center/organizational characteristics [59].
The improvement of survival may be attributed to advances in oncology [6, 7] and improved management of sepsis and related organ failure [60,61,62]. Thus, the prognosis of both patients with solid tumours and hematological malignancy has improved over time due to progress in management and new therapeutic options [6, 7]. In ICU, change in practices, prevention of deleterious consequences of mechanical ventilation, quick identification and management of sepsis have translated into improved in various groups of patients with acute kidney injury, sepsis or mechanical ventilation [60,61,62]. In addition, reports of poor outcomes of critically ill cancer patients in the literature might have led clinicians to forgo life-sustaining therapy early [63]. In a recent study, the authors were unable to confirm or exclude self-fulfilling prophecy effects and noted a tremendous difference across centers, driven by centers’ ethical climates [64]. It is important that clinicians are up to date with the literature to both improve clinical skills and willingness to care for critically ill cancer patients. Changes in clinicians’ perception of the prognosis of critically ill cancer patients may have contributed to changes in admission policy and management strategies and prevented inappropriate or premature decisions to withhold or withdraw life-sustaining therapies.
Only three of the tested subgroups did not experience a decrease in mortality over time. First, we were unable to demonstrate the improvement of survival in allogeneic HSCT recipients. We note that two recent large cohort studies suggested improved outcomes for this subgroup but in both cases, the results were unadjusted for potential confounders [14, 15]. The second subgroup where no change in mortality was detected were patients treated with renal replacement therapy. In critically ill non-cancer patients with acute kidney injury or requiring renal replacement therapy, a trend towards better outcomes has been reported [60, 65, 66] but there are no previous data from cancer patients admitted to the ICU. Changes in practice, including timing or indication of renal replacement therapy may have contributed to this finding but cannot be explored in our dataset. Our results suggest that more work is necessary. Last, we did not find any change in the outcome of patients who did not require mechanical ventilation. However, this subgroup is complex to delineate, being strongly influenced by ICU admission policy, bed availability and study inclusion criteria. Additional studies are needed to further explore these findings.
Our analysis has several important limitations. First, despite the biological plausibility, at best, we demonstrated a statistical association between survival and time. Factors explaining the association between ICU admission year and outcome were not addressed and need to be studied in more detail. Second, the observed associations are based on data from observational studies which may have been affected by allocation bias that was controlled for in our analysis. Accordingly, external validity of the included patients as well as hospital volume of cancer patients over time could not be approximated nor included in the analysis. However, to account for clustering effect and unrecorded confounders related to this later, a hierarchical model was used [67]. Such a bias along with changes in ICU admission policy would have, therefore, at least partly, been adjusted for. Similarly, patients’ severity of illness as assessed by severity scores and rate of organ support including vasopressors and mechanical ventilation, are similar to those of critically ill patients in general which suggests that selection bias and early ICU admission did not affect our findings [60,61,62]. Third, several variables, namely the use of granulocyte colony-stimulating factor (G-CSF) and neutropenia duration, were planned to be collected but were not consistently recorded in all studies. These variables were therefore dropped from the final analysis. Furthermore, the limited data on long-term outcome precluded analysis after short-term and namely hospital mortality. Thus, post-ICU mortality, after hospital mortality was not assessed and changed of these later may deserve to be tested in future studies. Last, in some subgroups, in particular in allogeneic HSCT recipients, the sample size was limited which decreased the statistical power of the analysis and should be kept in mind when interpreting the negative findings related to these subgroups.
In conclusion, this large cohort of individual data resulting from a systematic review, suggests progressive improvement of survival over time. The results were consistent across predefined subgroups except for allogeneic HSCT recipients, patients treated with renal replacement therapy, and patients who did not require mechanical ventilation. Our results support ICU admission of selected critically ill onco-hematological patients. When ICU admission is required, goals of care should be reviewed regularly to ensure the optimal delivery of therapy while avoiding inappropriate or futile care. Last, despite improved outcomes, additional studies are warranted to assess the impact of ICU admission policy, organizational factors and specific management strategies that may have contributed to these improvements.
Abbreviations
- DFLST:
-
Decision to forgo life-sustaining therapy
- ICU:
-
Intensive care unit
- HSCT:
-
Hematopoietic stem cell transplant
- OR:
-
Odds ratio
- RRT:
-
Renal replacement therapy
- IQR:
-
Interquartile range
- 95% CI:
-
95% Confidence interval
- APACHE:
-
Acute physiology and chronic health evaluation
- SAPS:
-
Simplified acute physiology score
References
Ferlay J, Soerjomataram I, Dikshit R et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359–E386. https://doi.org/10.1002/ijc.29210
GBD 2015 Mortality and Causes of Death Collaborators (2016) Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388:1459–1544. https://doi.org/10.1016/S0140-6736(16)31012-1
Vento S, Cainelli F, Temesgen Z (2008) Lung infections after cancer chemotherapy. Lancet Oncol 9:982–992. https://doi.org/10.1016/S1470-2045(08)70255-9
Morgan C, Tillett T, Braybrooke J, Ajithkumar T (2011) Management of uncommon chemotherapy-induced emergencies. Lancet Oncol 12:806–814. https://doi.org/10.1016/S1470-2045(10)70208-4
Wanchoo R, Karam S, Uppal NN et al (2017) Adverse renal effects of immune checkpoint inhibitors: a narrative review. Am J Nephrol 45:160–169. https://doi.org/10.1159/000455014
Brenner H (2002) Long-term survival rates of cancer patients achieved by the end of the 20th century: a period analysis. Lancet 360:1131–1135. https://doi.org/10.1016/S0140-6736(02)11199-8
Sant M, Minicozzi P, Mounier M et al (2014) Survival for haematological malignancies in Europe between 1997 and 2008 by region and age: results of EUROCARE-5, a population-based study. Lancet Oncol 15:931–942. https://doi.org/10.1016/S1470-2045(14)70282-7
Verdecchia A, Francisci S, Brenner H et al (2007) Recent cancer survival in Europe: a 2000–02 period analysis of EUROCARE-4 data. Lancet Oncol 8:784–796. https://doi.org/10.1016/S1470-2045(07)70246-2
Azoulay E, Recher C, Alberti C et al (1999) Changing use of intensive care for hematological patients: the example of multiple myeloma. Intensive Care Med 25:1395–1401
Peigne V, Rusinová K, Karlin L et al (2009) Continued survival gains in recent years among critically ill myeloma patients. Intensive Care Med 35:512–518. https://doi.org/10.1007/s00134-008-1320-4
Mokart D, Pastores SM, Darmon M (2014) Has survival increased in cancer patients admitted to the ICU? Yes. Intensive Care Med 40:1570–1572. https://doi.org/10.1007/s00134-014-3433-2
Darmon M, Azoulay E (2009) Critical care management of cancer patients: cause for optimism and need for objectivity. Curr Opin Oncol 21:318–326. https://doi.org/10.1097/CCO.0b013e32832b68b6
Shimabukuro-Vornhagen A, Böll B, Kochanek M et al (2016) Critical care of patients with cancer. CA Cancer J Clin 66:496–517. https://doi.org/10.3322/caac.21351
Lengliné E, Chevret S, Moreau A-S et al (2015) Changes in intensive care for allogeneic hematopoietic stem cell transplant recipients. Bone Marrow Transplant 50:840–845. https://doi.org/10.1038/bmt.2015.55
Lueck C, Stadler M, Koenecke C et al (2018) Improved short- and long-term outcome of allogeneic stem cell recipients admitted to the intensive care unit: a retrospective longitudinal analysis of 942 patients. Intensive Care Med 44:1483–1492. https://doi.org/10.1007/s00134-018-5347-x
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Bouteloup M, Perinel S, Bourmaud A et al (2017) Outcomes in adult critically ill cancer patients with and without neutropenia: a systematic review and meta-analysis of the Groupe de Recherche en Réanimation Respiratoire du patient d’Onco-Hématologie (GRRR-OH). Oncotarget 8:1860–1870. https://doi.org/10.18632/oncotarget.12165
Georges Q, Azoulay E, Mokart D et al (2018) Influence of neutropenia on mortality of critically ill cancer patients: results of a meta-analysis on individual data. Crit Care 22:326. https://doi.org/10.1186/s13054-018-2076-z
Rydenfelt K, Engerström L, Walther S et al (2015) In-hospital vs. 30-day mortality in the critically ill—a 2-year Swedish intensive care cohort analysis. Acta Anaesthesiol Scand 59:846–858. https://doi.org/10.1111/aas.12554
Schneider AG, Lipcsey M, Bailey M et al (2013) Simple translational equations to compare illness severity scores in intensive care trials. J Crit Care 28:885.e1–885.e8. https://doi.org/10.1016/j.jcrc.2013.02.003
Biard L, Labopin M, Chevret S et al (2018) Investigating covariate-by-centre interaction in survival data. Stat Methods Med Res 27:920–932. https://doi.org/10.1177/0962280216647981
Nattino G, Finazzi S, Bertolini G (2014) A new calibration test and a reappraisal of the calibration belt for the assessment of prediction models based on dichotomous outcomes. Stat Med 33:2390–2407. https://doi.org/10.1002/sim.6100
Poole D, Carrara G, Bertolini G (2017) Intensive care medicine in 2050: statistical tools for development of prognostic models (why clinicians should not be ignored). Intensive Care Med 43:1403–1406. https://doi.org/10.1007/s00134-017-4825-x
Azoulay E, Mokart D, Pène F et al (2013) Outcomes of critically ill patients with hematologic malignancies: prospective multicenter data from France and Belgium—a groupe de recherche respiratoire en réanimation onco-hématologique study. J Clin Oncol 31:2810–2818. https://doi.org/10.1200/JCO.2012.47.2365
Soares M, Salluh JIF, Carvalho MS et al (2006) Prognosis of critically ill patients with cancer and acute renal dysfunction. J Clin Oncol 24:4003–4010. https://doi.org/10.1200/JCO.2006.05.7869
Mokart D, Sannini A, Brun J-P et al (2007) N-terminal pro-brain natriuretic peptide as an early prognostic factor in cancer patients developing septic shock. Crit Care 11:R37. https://doi.org/10.1186/cc5721
Azoulay E, Mokart D, Rabbat A et al (2008) Diagnostic bronchoscopy in hematology and oncology patients with acute respiratory failure: prospective multicenter data. Crit Care Med 36:100–107. https://doi.org/10.1097/01.CCM.0000295590.33145.C4
McGrath S, Chatterjee F, Whiteley C, Ostermann M (2010) ICU and 6-month outcome of oncology patients in the intensive care unit. QJM 103:397–403. https://doi.org/10.1093/qjmed/hcq032
Legriel S, Marijon H, Darmon M et al (2010) Central neurological complications in critically ill patients with malignancies. Intensive Care Med 36:232–240. https://doi.org/10.1007/s00134-009-1709-8
Soares M, Silva UVA, Teles JMM et al (2010) Validation of four prognostic scores in patients with cancer admitted to Brazilian intensive care units: results from a prospective multicenter study. Intensive Care Med 36:1188–1195. https://doi.org/10.1007/s00134-010-1807-7
Song J-U, Suh GY, Chung MP et al (2011) Risk factors to predict outcome in critically ill cancer patients receiving chemotherapy in the intensive care unit. Support Care Cancer 19:491–495. https://doi.org/10.1007/s00520-010-0841-x
Bird GT, Farquhar-Smith P, Wigmore T et al (2012) Outcomes and prognostic factors in patients with haematological malignancy admitted to a specialist cancer intensive care unit: a 5 yr study. Br J Anaesth 108:452–459. https://doi.org/10.1093/bja/aer449
Hill QA, Kelly RJ, Patalappa C et al (2012) Survival of patients with hematological malignancy admitted to the intensive care unit: prognostic factors and outcome compared to unselected medical intensive care unit admissions, a parallel group study. Leuk Lymphoma 53:282–288. https://doi.org/10.3109/10428194.2011.614705
Xhaard A, Epelboin L, Schnell D et al (2013) Outcomes in critically ill chronic lymphocytic leukemia patients. Support Care Cancer 21:1885–1891. https://doi.org/10.1007/s00520-013-1744-4
Namendys-Silva SA, González-Herrera MO, García-Guillén FJ et al (2013) Outcome of critically ill patients with hematological malignancies. Ann Hematol 92:699–705. https://doi.org/10.1007/s00277-013-1675-7
Wohlfarth P, Staudinger T, Sperr WR et al (2014) Prognostic factors, long-term survival, and outcome of cancer patients receiving chemotherapy in the intensive care unit. Ann Hematol 93:1629–1636. https://doi.org/10.1007/s00277-014-2141-x
Soares M, Salluh JIF, Torres VBL et al (2008) Short- and long-term outcomes of critically ill patients with cancer and prolonged ICU length of stay. Chest 134:520–526. https://doi.org/10.1378/chest.08-0359
Depuydt PO, Benoit DD, Roosens CD et al (2010) The impact of the initial ventilatory strategy on survival in hematological patients with acute hypoxemic respiratory failure. J Crit Care 25:30–36. https://doi.org/10.1016/j.jcrc.2009.02.016
Canet E, Zafrani L, Lambert J et al (2013) Acute kidney injury in patients with newly diagnosed high-grade hematological malignancies: impact on remission and survival. PLoS One 8:e55870. https://doi.org/10.1371/journal.pone.0055870
Müller AM, Gazzana MB, Silva DR (2013) Outcomes for patients with lung cancer admitted to intensive care units. Rev Bras Ter Intensiva 25:12–16
Oeyen SG, Benoit DD, Annemans L et al (2013) Long-term outcomes and quality of life in critically ill patients with hematological or solid malignancies: a single center study. Intensive Care Med 39:889–898. https://doi.org/10.1007/s00134-012-2791-x
Ferrà C, Marcos P, Misis M et al (2007) Outcome and prognostic factors in patients with hematologic malignancies admitted to the intensive care unit: a single-center experience. Int J Hematol 85:195–202. https://doi.org/10.1532/IJH97.E0625
Soares M, Darmon M, Salluh JIF et al (2007) Prognosis of lung cancer patients with life-threatening complications. Chest 131:840–846. https://doi.org/10.1378/chest.06-2244
Toffart A-C, Minet C, Raynard B et al (2011) Use of intensive care in patients with nonresectable lung cancer. Chest 139:101–108. https://doi.org/10.1378/chest.09-2863
Burghi G, Lemiale V, Seguin A et al (2011) Outcomes of mechanically ventilated hematology patients with invasive pulmonary aspergillosis. Intensive Care Med 37:1605–1612. https://doi.org/10.1007/s00134-011-2344-8
Adda M, Coquet I, Darmon M et al (2008) Predictors of noninvasive ventilation failure in patients with hematologic malignancy and acute respiratory failure. Crit Care Med 36:2766–2772. https://doi.org/10.1097/CCM.0b013e31818699f6
Yoo H, Suh GY, Jeong B-H et al (2013) Etiologies, diagnostic strategies, and outcomes of diffuse pulmonary infiltrates causing acute respiratory failure in cancer patients: a retrospective observational study. Crit Care 17:R150. https://doi.org/10.1186/cc12829
Lee D-S, Suh GY, Ryu J-A et al (2015) Effect of early intervention on long-term outcomes of critically ill cancer patients admitted to ICUs. Crit Care Med 43:1439–1448. https://doi.org/10.1097/CCM.0000000000000989
Soares M, Salluh JIF, Toscano L, Dias FL (2007) Outcomes and prognostic factors in patients with head and neck cancer and severe acute illnesses. Intensive Care Med 33:2009–2013. https://doi.org/10.1007/s00134-007-0775-z
Souza-Dantas VC, Salluh JIF, Soares M (2011) Impact of neutropenia on the outcomes of critically ill patients with cancer: a matched case-control study. Ann Oncol 22:2094–2100. https://doi.org/10.1093/annonc/mdq711
Soares M, Toffart A-C, Timsit J-F et al (2014) Intensive care in patients with lung cancer: a multinational study. Ann Oncol 25:1829–1835. https://doi.org/10.1093/annonc/mdu234
Mokart D, Etienne A, Esterni B et al (2012) Critically ill cancer patients in the intensive care unit: short-term outcome and 1-year mortality. Acta Anaesthesiol Scand 56:178–189. https://doi.org/10.1111/j.1399-6576.2011.02579.x
Yeo CD, Kim JW, Kim SC et al (2012) Prognostic factors in critically ill patients with hematologic malignancies admitted to the intensive care unit. J Crit Care 27:739.e1–739.e6. https://doi.org/10.1016/j.jcrc.2012.07.014
Khassawneh BY, White P, Anaissie EJ et al (2002) Outcome from mechanical ventilation after autologous peripheral blood stem cell transplantation. Chest 121:185–188
Townsend WM, Holroyd A, Pearce R et al (2013) Improved intensive care unit survival for critically ill allogeneic haematopoietic stem cell transplant recipients following reduced intensity conditioning. Br J Haematol 161:578–586. https://doi.org/10.1111/bjh.12294
Zuber B, Tran T-C, Aegerter P et al (2012) Impact of case volume on survival of septic shock in patients with malignancies. Crit Care Med 40:55–62. https://doi.org/10.1097/CCM.0b013e31822d74ba
Benoit DD, Soares M, Azoulay E (2014) Has survival increased in cancer patients admitted to the ICU? We are not sure. Intensive Care Med 40:1576–1579. https://doi.org/10.1007/s00134-014-3480-8
Soares M, Bozza FA, Azevedo LCP et al (2016) Effects of organizational characteristics on outcomes and resource use in patients with cancer admitted to intensive care units. J Clin Oncol 34:3315–3324. https://doi.org/10.1200/JCO.2016.66.9549
Mokart D, Azoulay E, Schnell D et al (2013) Acute respiratory failure in neutropenic patients is associated with a high post-ICU mortality. Minerva Anestesiol 79:1156–1163
Bagshaw SM, George C, Bellomo R, ANZICS Database Management Committee (2007) Changes in the incidence and outcome for early acute kidney injury in a cohort of Australian intensive care units. Crit Care 11:R68. https://doi.org/10.1186/cc5949
Kaukonen K-M, Bailey M, Pilcher D et al (2015) Systemic inflammatory response syndrome criteria in defining severe sepsis. N Engl J Med 372:1629–1638. https://doi.org/10.1056/NEJMoa1415236
Esteban A, Frutos-Vivar F, Muriel A et al (2013) Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med 188:220–230. https://doi.org/10.1164/rccm.201212-2169OC
Lautrette A, Garrouste-Orgeas M, Bertrand P-M et al (2015) Respective impact of no escalation of treatment, withholding and withdrawal of life-sustaining treatment on ICU patients’ prognosis: a multicenter study of the Outcomerea Research Group. Intensive Care Med 41:1763–1772. https://doi.org/10.1007/s00134-015-3944-5
Benoit DD, Jensen HI, Malmgren J et al (2018) Outcome in patients perceived as receiving excessive care across different ethical climates: a prospective study in 68 intensive care units in Europe and the USA. Intensive Care Med 44:1039–1049. https://doi.org/10.1007/s00134-018-5231-8
Waikar SS, Curhan GC, Wald R et al (2006) Declining mortality in patients with acute renal failure, 1988 to 2002. JASN 17:1143–1150. https://doi.org/10.1681/ASN.2005091017
Xue JL, Daniels F, Star RA et al (2006) Incidence and mortality of acute renal failure in medicare beneficiaries, 1992 to 2001. JASN 17:1135–1142. https://doi.org/10.1681/ASN.2005060668
Panageas KS, Schrag D, Riedel E et al (2003) The effect of clustering of outcomes on the association of procedure volume and surgical outcomes. Ann Intern Med 139:658–665
Acknowledgements
The authors thank Sophie Perinel and Marie Bouteloup for their invaluable help with this study.
Funding
None.
Author information
Authors and Affiliations
Contributions
MD conceived the study, participated in study design and coordination, acquisition of data, statistical analysis and interpretation of data, drafting of the manuscript and critical revision of the manuscript. AB participated in statistical analysis, interpretation of data, drafting of the manuscript and critical revision of the manuscript. QG participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. MS participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. KJ participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. SO participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. CKR participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. PG participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. MO participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. QAH participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. PD participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. CF participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. ACT participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. PS participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. AM participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. VL participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. FT participated in statistical analysis, interpretation of data, drafting of the manuscript and critical revision of the manuscript. DM participated in study design, interpretation of data, and critical revision of the manuscript. EA participated in acquisition of data, interpretation of data, drafting of the manuscript and critical revision of the manuscript. All authors read and approved the final manuscript. MD affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as registered have been explained. MD had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Darmon report having received consulting fees from Sanofi and Gilead-Kite, research support from Astute Medical and MSD, and speaker fees from MSD, Gilead-Kite and Astellas. Dr Ostermann received research support from Fresenius Medical and LaJolla Pharma. Dr. Azoulay reports grants, personal fees and other from Gilead-Kite, personal fees from Baxter, personal fees and other from Alexion, grants from MSD, grants from Ablynx, non-financial support from Fisher & payckle, outside the submitted work. Other authors report no conflict of interest related to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Darmon, M., Bourmaud, A., Georges, Q. et al. Changes in critically ill cancer patients’ short-term outcome over the last decades: results of systematic review with meta-analysis on individual data. Intensive Care Med 45, 977–987 (2019). https://doi.org/10.1007/s00134-019-05653-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05653-7