Abstract
We reexamined the efficacy of Pathways early autism intervention using generalized measures of social communication and language skills administered by an unfamiliar adult in a novel environment. Generalized measures improve on sources of measurement bias. Sixty-seven autistic children blocked on age (under versus over 3 years) were randomly assigned to 15 weeks of Pathways or services-as-usual. Age moderated the effects of Pathways for social communication. Specifically, Pathways had a significantly large effect for children under 3 and a small effect that approached significance for children over 3. Pathways also had a small effect on expressive speech/language skills. Results replicate previous findings of the efficacy of Pathways on proximal and distal skills and support the importance of early intervention.
Similar content being viewed by others
Introduction
Autism spectrum disorder (ASD) is a complex, heterogeneous, neurodevelopmental disorder that severely compromises the development of social relatedness, reciprocity, social communication, joint attention, and learning. The Centers for Disease Control and Prevention estimated that 1 in 44 children are on the spectrum (Maenner et al., 2021). While a reliable diagnosis is possible between 18 and 24 months of age (Zwaigenbaum et al., 2015), the median age of diagnosis is between 3 and 4 years (Maenner et al., 2021). Early identification and intervention are crucial as the appropriate early intervention can support autistic childrenFootnote 1 in developing competencies in joint attention, social communication, and adaptive functioning (Fuller & Kaiser, 2020; Nahmias et al., 2019; Reichow, 2012; Schertz et al., 2012).
Naturalistic developmental behavioral interventions (NDBIs) are a class of empirically supported interventions appropriate for the needs of young autistic children. NBDIs blend social interactionist (Bruner, 1981; Snow, 1999; Vygotsky, 1978) and transactional approaches of development (Sameroff, 2009) with the science of applied behavior analysis to facilitate developmentally informed skills (Crank et al., 2021; Schreibman et al., 2015). Parent-mediated NDBIs, in which caregivers are coached to implement intervention strategies within the child’s daily interactions, are associated with positive effects for social, communication, and language skills (Brian et al., 2017; Kasari et al., 2015; Rollins et al., 2021; Siller et al., 2013; Wetherby et al., 2018). Parent-mediated NBDIs can be delivered in a manner consistent with the Individuals with Disabilities Education Act (IDEA) Part C Early Childhood Intervention (ECI) programs (Rollins et al., 2021; Wetherby et al., 2018). Part C is a federal grant program that assists states in operating statewide community programs for infants and toddlers with disabilities. These programs necessitate the provision of family-centered and family capacity-building practices that enhance the family’s ability to promote the child’s development within authentic learning experiences (Adams et al., 2013; Division for Early Childhood of the Council for Exceptional Children [DEC], 2014; Schertz et al., 2011).
Recently, Rollins et al. (2016, 2021) examined the efficacy of Pathways Early Autism Intervention (Pathways) on social development. Pathways is a parent-mediated NDBI that fits the service delivery model of IDEA Part C programs in Texas and other low-resourced states. Pathways is a low-dose (1.5 h per week), manualized, parent-mediated NDBI. Pathways interventionists coach caregivers to follow their child’s lead, use wait time, limit distractions and demands, and engage in face-to-face positioning, mutual gaze, animation, and imitation. Many of these strategies are found in other researched-based NDBIs (Brian et al., 2017; Ingersoll & Gergans, 2007; Kasari et al., 2015; Koegel et al., 2009; Wallace & Rogers, 2010; Wetherby et al., 2018). However, Pathways differs from other interventions in that caregivers are coached to actively engage their child in mutual gaze. Mutual gaze is an essential component of early dyadic interaction in infants with typical development that may activate the social brain network (Johnson et al., 2015; Jones & Klin, 2013; Mundy & Bullen, 2022; Senju & Johnson, 2009). Unlike infants developing typically, autistic infants exhibit a decline in eye gaze between two and six months, suggesting they miss out on opportunities to engage in mutual gaze and fundamental social interactions. Interventions that target mutual gaze, such as Pathways, may adjust the pattern of brain activity toward a more social trajectory (Johnson et al., 2015; Jones & Klin, 2013; Mundy & Bullen, 2022; Senju & Johnson, 2009).
Rollins et al. (2021) randomized ECI-aged toddlers into a Pathways, communication, or a services-as-usual group (SAU). The communication intervention was identical to Pathways, except caregivers were coached on strategies to facilitate communication instead of mutual gaze, and the SAU group received community-based early intervention. The comparison with the communication group found Pathways to have significant medium effects on social skills and adaptive functioning but no effect on communication (Table 1). These findings support that mutual gaze is pivotal for social development and has cascading influences on communication and adaptive functioning (Johnson et al., 2015; Jones & Klin, 2013; Mundy, 2016; Mundy & Bullen, 2022), at least in ECI-aged children. Compared to the SAU group, Pathways had significantly large effects on social and adaptive functioning and a medium effect on communicative synchrony. In addition, using an overlapping sample, Rollins et al. (2019) found that Pathways had significantly large effects on improving caregiver responsivity and decreasing caregiver stress compared with community-based early intervention (Table 1). The large effects on child and caregiver functioning suggest that Pathways may be an effective ECI intervention.
Unfortunately, the median age of diagnosis for autistic children is between 3 and 4 years (Maenner et al., 2021), when autistic children are no longer eligible for Part C ECI services. ECI capitalizes on experience-dependent neuroplasticity changing the quality and quantity of interactions that may be disrupted (Landa, 2018). The developmental processes involved in the social brain network may be less malleable over time (Johnson et al., 2015; Landa, 2018) suggesting that as autistic children age, they may be less able to realize the benefits of intervention (Dawson, 2008; Landa, 2018). Further, recent metanalyses have found that the effect of age on intervention may differ by outcome variable (Sandbank, Bottema-Beutel, Crowley, Cassidy, Feldman, et al., 2020) with social outcomes being more susceptible to age effects (Fuller & Kaiser, 2020; Gabbay-Dizdar et al., 2021) than spoken language (Hampton & Kaiser, 2016). Therefore, it is essential to identify if Pathways continues to be effective for gains in social development for autistic children who are older than 36 months of age.
It is also important to note that all measures used in the Pathways studies were obtained during caregiver-child interactions (CCI) or by standardized caregiver interviews (Table 1), which may have inflated the intervention effects (Fuller & Kaiser, 2020; Yoder et al., 2013). First, caregivers in the intervention group had the advantage of implementing facilitative strategies learned during the intervention, whereas caregivers in the control group did not (Yoder & Crandall, 2019). Because the resulting measures of social and communication skills may be influenced by caregiver facilitative techniques, measurement constancy (i.e., measuring a construct the same way in both groups) was not attained (Sandbank, Bottema-Beutel, Crowley, Cassidy, Dunham, et al., 2020, Sandbank, Bottema-Beutel, Crowley, Cassidy, Feldman, et al., 2020; Yoder & Crandall, 2019). Second, because a caregiver provides the parent-mediated intervention, outcome measures are extracted from the same context as the intervention (i.e., context boundedness). It is unknown if the results generalize to other settings or unfamiliar adults interacting with the children (Yoder & Crandall, 2019). Third, caregivers may experience a positive emotional response to learning new skills and providing the intervention, which may bias caregivers’ ratings during interviews following the intervention (a placebo by proxy effect, Grelotti & Kaptchuk, 2011) and increase the correlated measurement error (Crank et al., 2021; Sandbank, Bottema-Beutel, Crowley, Cassidy, Dunham, et al., 2020, Sandbank, Bottema-Beutel, Crowley, Cassidy, Feldman, et al., 2020). It is essential to redress these measurement issues to understand Pathways’s effects on social development in young autistic children.
The purpose of the present study is twofold. The first is to examine the efficacy of Pathways on social communication, expressive speech/language, and symbolic behaviors using a measure administered by an unfamiliar adult in a clinic environment. Unlike our previous studies, a generalized measure of social communication, expressive speech, and symbolic behavior will allow us to improve on correlated measurement error, measurement constancy, context boundedness, and the generalizability of these skills. The second is to examine if the efficacy of Pathways differs in children 3–4 years of age who are eligible for part B services from toddlers who are younger than 3 years and eligible for ECI services from IDEA Part C.Footnote 2 In the current study, the Pathways group is compared with a SAU control group that received services from public and private community organizations. Of note, the participants in the present research are independent from participants from previous Pathways studies.
We anticipate replicating previous findings on the efficacy of Pathways for children under 3 and thus hypothesize that children in the Pathways group will demonstrate significantly greater gains in social communication skills and similar gains in expressive speech and symbolic behaviors compared to the SAU group. We further hypothesize that Pathways’s effect on social communication will not wane in 3–4-year-olds. Although previous studies suggest the efficacy of intervention on social outcomes may vary by age (Sandbank, Bottema-Beutel, Crowley, Cassidy, Dunham et al., 2020, Sandbank, Bottema-Beutel, Crowley, Cassidy, Feldman, et al., 2020), Pathways’s focus on incorporating mutual gaze within early developing dyadic interactions may continue to adjust the pattern of early social development towards a more social trajectory in 3–4-year-old children.
Methods
Participants
Caregivers and children aged 18 to 50 months were recruited through local infant toddler programs, community centers, advocacy groups, physicians’ offices, social media, and word of mouth. Eligibility criteria included: (a) having a chronological age of less than 50 months at the start of the study; (b) receiving an autism spectrum classification on the Autism Diagnostic Observation Schedule, Second Edition (ADOS-2; Lord et al., 2012), administered by an ADOS-2 reliable examiner; (c) having no other known medical, neurological, or genetic concerns or disorders; and (d) having a primary home language of English or Spanish.
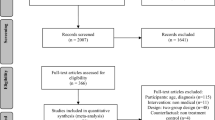
Of the 97 children initially assessed, sixty-nine children met inclusion criteria prior to the COVID-19 Pandemic (Fig. 1). Eight families who finished the intervention could not receive post-intervention assessments due to the COVID-19 pandemic (i.e., sheltering-in-place orders followed by cessation of human subjects research). An additional 12 families did not complete the intervention or receive post-assessment because they had a prolonged illness, death in the family, moved out of the area/country, or could not be reached to schedule post-intervention assessments. Two children were not included in the analysis for the present study because they were functioning above the age at which the Communication and Symbolic Behavior Scales- Developmental Profile (CSBS DP; Wetherby & Prizant, 2002) is a valid measure (see CSBS DP measure below). Attrition analyses were based on What Works Clearinghouse (WWC) attrition standards (What Works Clearinghouse [WWC], 2020) for rating RCT with missing outcome data. The WWC attrition model evaluates potential bias as a function of overall and differential attrition rates. Sample loss due to nature such as the COVID-19 pandemic need not be counted as attrition, however, we included those children in the analyses. The attrition rates for both the Pathways and the SAU groups were 31%, yielding a differential attrition rate of 0%. Consequently, the combination of the overall (31%) and differential (0%) attrition rates generated a tolerable expected bias level. Accordingly, WWC (2020) rates bias due to sampling attrition as low.
Baseline child and family characteristics are presented in Table 2. Notably, the sample is independent from the sample used in previous Pathways efficacy studies. Demographics (race/ethnicity and family income) show substantial diversity relative to most existing autism research and are broadly representative of that of Dallas County, Texas, with the exception that our sample contains a larger percentage of Asian and a lower percentage of Black/African American participants (United States Census Bureau, n.d.). Twenty-one participants reported speaking Spanish most or all of the time at home. The children, on average, had significant cognitive and linguistic delays and high levels of autism symptomatology. All caregivers consented to the study using an informed consent procedure approved by the university’s Institutional Review Board.
Study Design
This study used a stratified simple random sample with a waitlist control design and intent-to-treat (ITT) analyses. ITT models are based on group assignment and do not include corrections for participant loss due to attrition. Families were randomized in a 1:1 allocation by IDEA Part B and C eligibility groups (i.e., older than 3 years versus younger than 3 years). The principal investigator used a computer-generated list of random numbers to allocate participants to treatment conditions and sealed envelopes for allocation concealment. Researchers opened the envelopes after families completed all baseline assessments. Clinical researchers administered the assessments and provided the intervention for the Pathways group. Consequently, interventionists were blind to group assignment at baseline but not post-intervention. An interventionist not familiar with the family conducted post-intervention assessments to minimize bias. Recruiting, intake, and pre-and post-intervention testing procedures were identical for both conditions. The Pathways group received up to 12 project-related home visits within 15 weeks. The SAU control group received 15 weeks of services as usual from community-based early intervention providers. Families in the SAU control group could elect to receive the Pathways intervention at no charge when they completed the study.
Interventionist Qualifications
Six clinical researchers were responsible for administering the assessments and providing the intervention. Three were bilingual (English/Spanish) and provided assessments and interventions in Spanish when Spanish was the primary language of the home. Interventionist qualifications and training are detailed in Rollins et al. (2021). Interventionists were trained on Pathways to fidelity, using practice children prior to the start of the study. In addition, they participated in weekly supervision with the first author where they reviewed and discussed video recordings of treatment sessions. No other procedural fidelity measures were obtained.
Pathways Intervention
The Pathways intervention is a targeted, manualized program with English and Spanish versions of the manuals available in print and digitized audio formats. Caregivers received family-centered coaching for 1.5 h per week, using adult learning methods that foster active learning within authentic settings to enhance the family's capacity to promote their child's development (DEC, 2014; Dunst & Trivette, 2012; Friedman et al., 2012; Rush & Shelden, 2011). Coaching methods include multimodal methods to disseminate information, demonstration, practice, in vivo feedback/guidance, self-reflection, and evaluation. The intervention is incremental, with each unit building on the preceding unit. Therefore, once a caregiver learns a strategy, they use it with the child for the remaining weeks of the intervention. The units focus in succession on following the child's lead, using wait time, limiting distractions and demands, face-to-face positioning, mutual gaze, animation, and imitation (Table 3). Caregivers are encouraged to use the interactional strategies throughout much of their child's day by utilizing play activities and social sensory and daily routines appropriate to each family's culture.
Pathways differs from other interventions in that caregivers are coached to engage their child in mutual gaze. Interventionists typically introduce mutual gaze in week 3 or 4 of the 15-week intervention. Initially, caregivers actively capture the child's eye gaze during a motivating social sensory routine when the child is not socially orienting to the caregiver’s gaze. Once the caregiver establishes eye gaze, they provide the child with contingent natural reinforcement by continuing the routine. Notably, the strategy requires the caregiver to actively capture the child's eye gaze without verbal, visual, or physical prompts. As the practice becomes established, the caregiver uses wait time to allow the child to spontaneously social orient to continue the routine. Later, as the practice expands, caregivers are encouraged to hold the child's eye gaze for extended periods, pausing the routine when the child looks away. The interaction evolves with the child engaging in several rounds of social orienting followed by mutual gaze for all or most of the routine. See Rollins et al. (2021) for additional details regarding intervention and coaching.
Caregiver Implementation Fidelity
Each week, interventionists rated caregiver implementation fidelity for each strategy on a scale of 1 to 4 (3 = strategy implemented correctly; 4 = caregiver is natural at implementing strategy). An average fidelity score was calculated for each caregiver. Overall average caregiver fidelity was high (M = 3.6, SD = 0.3, range = 2.95 – 3.96) and 96% of caregivers obtained an average fidelity rating of 3.0 or greater.
Measures
Clinical researchers collected assessments at baseline before randomization and again at post-intervention in either English or Spanish, depending on the child's primary language. Assessments were administered within two weeks of the start and stop of the intervention phase at a Callier Center for Communication Disorders location that was most accessible for the family. Clinical researchers were blind to group assignment at baseline but not post-intervention. Instead, a clinical researcher not familiar with the family conducted the post-intervention assessments to minimize bias.
ASD Classification
The ADOS-2 was administered prior to randomization to confirm a research diagnosis of ASD. The ADOS-2 is a semi-structured evaluation of communication, social interaction, play, and restricted/repetitive behaviors for children suspected of having ASD. The ADOS-2 has been used successfully with Spanish-speaking autistic children (Ohashi et al., 2012; Stronach & Wetherby, 2017). The ADOS-2 is available in five versions (modules) selected based on the child’s age and expressive language level. For the present study, a researcher who was trained on site to be ADOS-2 reliable administered the ADOS-2. The Toddler Module, intended for children 12–30 months of age, was administered to 26 children. Module 1 of the ADOS-2, intended for children aged 31 months and older whose language abilities range from no speech to simple phrases, was administered to 41 children. All ADOS-2 scores were converted to Calibrated Severity Scores (CSS) to allow comparisons across modules.
Receptive Language
The Mullen Scales of Early Learning (MSEL; Mullen, 1995) was administered prior to randomization to estimate receptive language. The MSEL is a standardized, direct assessment of development for young children (aged 0–68 months) that yields age-equivalency scores for gross and fine motor skills, visual reception, and receptive and expressive language. Age equivalency scores were used to measure receptive language. These scores are commonly reported in studies on ASD, which enhances comparability across studies (Sandbank, Bottema-Beutel, Crowley, Cassidy, Dunham, et al., 2020, Sandbank, Bottema-Beutel, Crowley, Cassidy, Feldman, et al., 2020). Notable, there is not a Spanish version of the MSEL. Consequently, developmental quotients were not calculated for this study. We found high correlations for language scores between the MSEL and the Spanish version of the Vineland Adaptive Behavior Scales, Second Edition (VABS; Sparrow et al., 2005) for the children whose primary language was Spanish (r = 0.85 p < 0.001 for receptive language) thereby increasing the criterion validity of the MSEL receptive language scores for these children.
Adaptive Functioning
The English or Spanish version of the caregiver interview form of the VABS was administered prior to randomization and post-intervention to measure child adaptive functioning skills. Only pre-intervention scores were used in the current study. Pre-intervention scores are less subject to placebo by proxy effects as participants have not yet been randomized to an intervention group. The VABS is a standardized test of adaptive functioning for individuals from birth to age 90. The test yields an adaptive behavior composite score and domain scores for communication, daily living, socialization, and motor development and has good test–retest reliability (0.88–0.92).
Social Communication, Expressive Speech/Language, and Symbolic Skills
The CSBS DP was administered prior to randomization and at post-intervention. The CSBS DP is a direct assessment designed to assess early social communication, expressive speech/language and symbolic behaviors in children 6 months to 6 years whose functional communication and symbolic behavior is commensurate with typically developing children aged 6 months to 2 years. Children in the current study all scored within or below the average range for two-year-old children on the CSBS DP total score, confirming functional communication and symbolic behavior was within the range appropriate for this assessment. The CSBS DP yields composite scores for Social, Speech, and Symbolic skills (raw scores were used in the present analyses because they are strictly comparable across time points). The Social Composite measures social communication and is comprised of three subscales: social emotional signaling and joint attention, gestures, and communication. The Speech Composite measures expressive speech/language and is comprised of two subscales: sounds and words. Finally, the Symbolic Composite measures symbolic skills and is comprised of two subscales: understanding and object use. The CSBS DP has good internal consistency (0.86 to 0.89) and test–retest reliability (0.77 to 0.93; Wetherby & Prizant, 2002) and has been used successfully with Spanish-speaking autistic children (Stronach & Wetherby, 2017).
Data Analytic Strategy
IBM SPSS statistical package version 27 and SAS OnDemand release 9.04.01 were used to analyze the data. First, we provide descriptive statistics and preliminary analyses to establish pre-intervention group equivalencies on all baseline characteristics found in Table 2. T-tests were used to test for group equivalencies for the continuous measures, and Chi square analyses were used for the categorical variables.
Attrition analysis (described above) found the bias due to sampling attrition is rated as low (WWC, 2020). Therefore, multiple imputations is considered an appropriate method of handling our analyses (WWC, 2020). Specifically, to address the problem of non-monotone missing data we performed multiple imputation using the Markov-chain Monte Carlo (MCMC) method under the assumptions of multivariate normality and missing at random (MAR). It is noteworthy that the MAR assumption is not testable, however, including auxiliary variables that are correlated with our outcome measures makes the MAR assumption more plausible and increases the efficiency of the estimates (Allison, 2009). Following recommended practice, we included interaction and dependent variables as auxiliary variables (Allison, 2009; Manly & Wells, 2015). Auxiliary variables for all models were: Group, AGE, the Group x AGE interaction, mother’s education in years, average non-project therapy hours, ADOS-2 Social CSS, ADOS-2 Total CSS, MSEL receptive language age in months, Time 1 VABS expressive language raw scores, Time 1 VABS Communication composite raw scores, Time 1 VABS Social domain raw score, Time 1 VABS adaptive behavior composite, and Time 1 and 2 CSBS total raw scores. In addition, for each outcome variable (CSBS Social, CSBS Speech, and CSBS Symbolic), the respective Time 1 and Time 2 CSBS raw scores were also added as auxiliary variables.
We calculated descriptive statistics for pre-and post-intervention CSBS DP raw scores on imputed data from the SAS PROC MI command. The BY _IMPUTATION_ statement in the SAS PROC UNIVARIATE procedure generated 25 imputed datasets combined using SAS PROC MIANALYZE. Similarly, analyses for each outcome were performed using regression analyses on imputed data from the SAS PROC MI command. For each regression analysis, the BY _IMPUTATION_ statement in the SAS PROC REG command generated 25 imputed datasets combined using SAS PROC MIANALYZE. We compared results from the multiple imputations analyses with those obtained using listwise deletion (Online Resource 1) and found no discrepancies. Therefore, following the recommendation by Manly and Wells (2015), only imputed results are presented.
To test whether AGE moderated the efficacy of Pathways we used regression analyses, simultaneously entering the pre-intervention CSBS DP measure, the dummy-coded group variable, a dummy-coded AGE variable comparing between ECI eligibility groups (older than 3 years versus younger than 3 years) and the Group x AGE interaction variable. When the interaction variable was significant, we conducted follow-up analyses probing the interaction (Hayes, 2018). When the interaction variable was not significant, we used hierarchical regression entering each variable one at a time into the model. The coefficient of determination (i.e., R2) and change in R2 (i.e., ΔR2) were calculated using the average R2 on the 25 imputed regression models (van Ginkel, 2019). The partial f-statistic was used to determine the statistical significance for the change in R2 (i.e., ΔR2) for each question variable entered. Effect-size estimates were assessed by the magnitude of the effect obtained from the R2 or ΔR2. The specific effect size calculation was f2 = R2/1 – R2, and interpretation was based on Cohen (1992), where f2 ≥ 0.02 suggests a small effect; ≥ 0.15, a medium effect; and ≥ 0.35, a large effect. All assumptions of regression were analyzed. No model violations were present when log variables were entered.
Power Analysis
G*Power (Faul et al., 2007) was used to conduct sensitivity power analyses given α = 0.05 and power (1 − β) = 0.80. For an interaction with two dichotomous variables, results indicated a medium-to-large effect could be detected with our achieved sample size of 67 (f = 0.34). For R2 increment testing in a fixed model linear regression with two test predictor and between two and five total predictors, results indicated a medium effect could be detected given our sample size (f2 = 0.15).
Results
Preliminary Analyses
Pretreatment group equivalencies were analyzed using t-tests for continuous variables and Chi-Square test for categorical variables. There were no significant group differences on baseline variables. Medium effects were noted for receptive language age and adaptive behavior (Table 2). Means and standard deviations for Pathways and SAU pre- and post-intervention CSBS DP raw scores are presented in Table 4 (see Online Resource 2 for results using listwise deletion).
Social Communication
We found that AGE significantly moderated the effects of Pathways on Time 2 CSBS social communication, adjusting for CSBS social communication at Time 1 (b = − 8.17, t(4,62) = − 2.05, p = 0.04, 95% CI − 15.98, − 0.36). The moderation model accounted for 67% (R2 = 0.67) of the variation in Time 2 social communication, which is a large effect (f 2 = 2.03). Probing the interaction (Fig. 2), we found the conditional effect of group on Time 2 social communication was significant for children under 3 years of age but not for children over age 3. Specifically, there was, on average, a 13.67-point difference between Pathways and SAU for children under 3 (b = 13.67, t(4,62) = 5.21, p = 0.04, 95% CI 8.53, 18.81), but only a 5.51-point difference between the groups for children over 3 (b = 5.51, t(4,62) = 1.73, p = 0.08, 95% CI − 0.75, 11.76). As would be expected from the magnitude of the unstandardized beta coefficients, the effect size of Pathways on Time 2 social communication (adjusting for Time 1 social communication) was large for children under 3 (f 2 = 0.40; ΔR2 = 0.29, F(1,38) = 19.8, p < 0.001) and small for children over 3 (f 2 = 0.07; ΔR2 = 0.07, F(1,24) = 3.61, p = 0.06).
Expressive Speech/Language
AGE did not moderate the effect of group on expressive language. Hierarchical regression models for expressive speech/language are found in Table 5. Model 1 is the base model that contains pre-intervention expressive speech/language skills. Model 2 tested the effects of group and Model 3 AGE. The results suggest that adjusting for the pre-intervention expressive speech/language, the Pathways group had significantly higher expressive speech/language skills post-intervention and the magnitude of the effect was small (f2 = 0.04). There was not a significant difference for AGE.
Symbolic Skills
AGE did not moderate the effect of group on symbolic skills. Further, adjusting for pre-intervention symbolic behavior there was not a significant difference between the Pathways and SAU groups nor was there a significant difference for AGE.
Discussion
Pathways is a parent-mediated NDBI that fits the guiding principles and service delivery model of IDEA Part C programs in low-resourced states. Pathways differs from other NBDIs in that caregivers are coached to engage their child in mutual gaze within dyadic interactions. Mutual gaze is a focus of intervention because it may be pivotal for social development with cascading effects on other areas of development (Rollins et al., 2021; Mundy & Bullen, 2022). Compared to children in community-based programs, previous studies found Pathways to have large effects on early social development and adaptive functioning, medium effects on communicative complexity and no effect on the number and diversity of communicative acts in Part C-aged children (Rollins et al., 2021). The previous research used caregiver report measures and context-bound caregiver-child interaction measures to assess efficacy. Noteworthy, research assistants coding caregiver-child interactions were blind to group assignment and pre- versus post-intervention status, reducing detection bias. However, using caregivers as agents of the assessments may have inflated the intervention effects because of correlated measurement error, violations of measurement constancy, and context boundedness, limiting statements about the generalizability of skills. To combat these potential biases, we utilized a standard assessment procedure administered in a novel environment by a clinical researcher unfamiliar with the child in the present study. In addition, we examined if Pathways continues to be effective for children over 3 years (who are served by IDEA Part B services). Despite differences in participants, measurement, and age, we hypothesized that we would replicate the previous findings for children under 3-year and that the results would not differ for children older than 3-years who are no longer eligible for IDEA Part C services.
We found that Pathways had a large effect on social communication for ECI-aged autistic children. The effect size with our generalized measure of social communication is consistent with previous research that used context-bound caregiver–child and caregiver-report measures. However, all measures of social skill, including the CSBS Social composite, are proximal measures because Pathways targets early-developing dyadic social skills. Nevertheless, social delays are a core feature of ASD, making it critical to support autistic children in developing social competencies generalizable to unfamiliar communication partners (Crank et al., 2021).
Contrary to our hypothesis, we found that AGE moderated the effects of Pathways on social communication. Specifically, Pathways had a significant and large effect for children under age 3 and a small effect that approached significance for children over age 3. On average, the difference in Time 2 CSBS Social scores between the Pathways and SAU groups for ECI-aged children was 13.67. The difference decreased by 8.17 points, on average, in children over 3 who are eligible for Part B services. Notably, a limitation of this study is related to power, and we were not powered to detect the small effect of a 5.51-point difference between the groups for the older age. Nevertheless, the effect for children over 3 approached significance and may have practical significance.
Our results are consistent with previous findings that chronological age moderates the effects of an intervention on the social skills of autistic children (Fuller & Kaiser, 2020; Gabbay-Dizdar et al., 2021) and underscore the necessity for early intervention services. However, it is unclear why the degree of benefit from intervention on social skills decreases with age. One hypothesis is that the social brain network becomes less malleable over time, diminishing the effects of experience-dependent neuroplasticity (Johnson et al., 2015; Landa, 2018). Alternatively, there may be a developmental window during which mutual gaze optimizes social development, and a shift in intervention strategies focusing on interactions to promote joint attention (Shire et al., 2016) may be necessary as the child ages.
A related hypothesis is that children over the age of 3—who are eligible for public school services—may spend less time interacting with their caregivers than children under the age of 3. Consequently, the intervention dosage may have been much less for the older children. Future research for children over 3 should include a team approach combining caregivers and school-based clinicians as Pathways interventionists (Fuller & Kaiser, 2020; Landa, 2018). Further, a comparison between a mutual gaze and a joint attention intervention could identify if changes to the intervention agent and intervention type impact social development in children over 3.
Also, contrary to our hypothesis, children in the Pathways group made significant gains in expressive speech/language skills. However, as expected from an outcome more distal to the intervention targets, the effect was small. Unfortunately, we were not powered to detect if AGE moderated expressive speech/language effects. While an age interaction is plausible, expressive speech/language may be less susceptible to AGE effects than social communication (Crank et al., 2021; Hampton & Kaiser, 2016). Nonetheless, the finding is meaningful because expressive speech/language skills are a common focus of SAU interventions in our community but not a target of Pathways. Further, the effect on this distal outcome suggests a cascading effect of mutual gaze within early dyadic interactions on expressive speech/language skills.
Finally, we did not find Pathways effective for symbolic skills. The null effect was not surprising because Pathways focuses on early dyadic interactions observed between caregivers and infants developing typically around 2 to 6 months of age rather than later developing triadic interactions needed for symbolic play. In addition, the children were largely developmentally prior to possessing the social skills needed for coordinating joint attention with another person at the study's completion. Because mutual gaze within early dyadic social interactions is a putative precursor of joint attention (Adamson & Russell, 1999; Tomasello et al., 2005), we anticipate that a more extended intervention period would build toward triadic interactions and provide sufficient time to develop more complex social communication skills.
While there are several strengths to this study, including a culturally diverse sample and generalized measures, there remain several methodological limitations. As stated above, a limitation of this study is power which may have contributed to Type II errors (i.e., failing to reject the null hypothesis when the null hypothesis is false) with regards to the small effect of Pathways on social communication for children over 3 and not realizing a moderation effect for expressive speech and language. Another limitation is that the clinical researchers who administered the CSBS DP assessments were not blind to the intervention group post-intervention, creating a risk of detection bias (Sandbank, Bottema-Beutel, Crowley, Cassidy, Dunham, et al., 2020; Sandbank, Bottema-Beutel, Crowley, Cassidy, Feldman, et al., 2020). However, a clinical researcher unfamiliar with the child and family administered post-intervention assessments to mitigate potential bias. A third limitation is a lack of follow-up data 3- and 6-months post-intervention to determine whether the effects are sustainable. Unfortunately, the negative impact of the COVID-19 pandemic on our follow-up data was substantial, and we could not rectify the data loss with multiple imputation for non-monotone missing data. Finally, the short duration of the intervention did not allow sufficient time for the children to develop more complex social communication skills. Future research, for children under 3 should extend the duration of intervention to examine if more advanced social skills can be realized and include follow-up data 3- and 6-months post-intervention to assess if the effects are sustainable or if there are delayed effects on distal outcomes (Crank et al., 2021).
Despite these limitations, the results of the present study highlight the efficacy of Pathways as an early autism intervention for ECI-aged children. The use of generalized outcome measures that differed from the intervention with regards to communication partner improved on several sources of measurement bias (Crank et al., 2021). When compared with community-based SAU, the ECI aged children in the Pathways group exhibited more progress in social communication skills (large effect) and expressive speech/language (small effect) and similar progress in symbolic (receptive language and play) skills. Our finding that Pathways has effects on outcomes distal to the intervention suggests that mutual gaze within dyadic interactions has a cascading effect on the development of expressive speech and language for young cognitively and linguistically delayed autistic children. These findings are of particular importance as two goals of NDBIs are to promote generalization and to realize cascading effects of an intervention on distal areas of development (Crank et al., 2021; Schreibman et al., 2015), further underscoring the efficacy of Pathways as a parent-mediated NDBI for children under 3 years of age.
Notes
Identity-first language will be used as it has been found to be generally preferred by autistic individuals (Bottema-Beutel et al., 2021).
IDEA Part C (ECI) serves children until their third birthday; on and after their third birthday, children are served by IDEA Part B.
References
Adams, R. C., Tapia, C., Murphy, N. A., Norwood, K. W., Burke, R. T., Friedman, S. L., Houtrow, A. J., Kalichman, M. A., Kuo, D. K., Levy, S. E., Turchi, R. M., Wiley, S. E., The Council on Children with Disabilities. (2013). Early intervention, IDEA Part C services, and the medical home: Collaboration for best practice and best outcomes. Pediatrics, 132(4), e1073–e1088. https://doi.org/10.1542/peds.2013-2305
Adamson, L. B., & Russell, C. L. (1999). Emotion regulation and the emergence of joint attention. In P. Rochat (Ed.), Early social cognition: Understanding others in the first months of life (pp. 281–295). Erlbaum.
Allison, P. D. (2009). Missing Data. In R. E. Milsap & A. Maydeu-Olivares (Eds.), The SAGE handbook of quantitative methods in psychology (pp. 72–89). Sage Publications Inc.
Bottema-Beutel, K., Kapp, S. K., Lester, J. N., Sasson, N. J., & Hand, B. N. (2021). Avoiding ableist language: Suggestions for autism researchers. Autism in Adulthood. https://doi.org/10.1089/aut.2020.0014
Brian, J. A., Smith, I. M., Zwaigenbaum, L., & Bryson, S. E. (2017). Cross-site randomized control trial of the Social ABCs caregiver-mediated intervention for toddlers with autism spectrum disorder. Autism Research, 10(10), 1700–1711. https://doi.org/10.1002/aur.1582
Bruner, J. S. (1981). The social context of language acquisition. Language & Communication, I(2–3), 155–178. https://doi.org/10.1016/0271-5309(81)90010-0
Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159. https://doi.org/10.1037/0033-2909.112.1.155
Crank, J. E., Sandbank, M., Dunham, K., Crowley, S., Bottema-Beutel, K., Feldman, J., & Woynaroski, T. G. (2021). Understanding the effects of naturalistic developmental behavioral interventions: A project AIM meta-analysis. Autism Research, 14(4), 817–834. https://doi.org/10.1002/aur.2471
Dawson, G. (2008). Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Development and Psychopathology, 20(3), 775–803. https://doi.org/10.1017/S0954579408000370
Division for Early Childhood of the Council for Exceptional Children. (2014). DEC recommended practices in early intervention/early childhood special education 2014. Retrieved from http://www.dec-sped.org/recommendedpractices
Dunst, C. J., & Trivette, C. M. (2012). Moderators of the effectiveness of adult learning method practices. Journal of Social Sciences, 8(2), 143–148.
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/bf03193146
Friedman, M., Woods, J., & Salisbury, C. (2012). Caregiver coaching strategies for early intervention providers: Moving toward operational definitions. Infants & Young Children, 25(1), 62–82. https://doi.org/10.1097/IYC.0b013e31823d8f12
Fuller, E. A., & Kaiser, A. P. (2020). The effects of early intervention on social communication outcomes for children with autism spectrum disorder: A meta-analysis. Journal of Autism and Developmental Disorders, 50(5), 1683–1700. https://doi.org/10.1007/s10803-019-03927-z
Gabbay-Dizdar, N., Ilan, M., Meiri, G., Faroy, M., Michaelovski, A., Flusser, H., Menashe, I., Koller, J., Zachor, D. A., & Dinstein, I. (2021). Early diagnosis of autism in the community is associated with marked improvement in social symptoms within 1–2 years. Autism. https://doi.org/10.1177/13623613211049011
Grelotti, D. J., & Kaptchuk, T. J. (2011). Placebo by proxy. BMJ. https://doi.org/10.1136/bmj.d4345
Hampton, L. H., & Kaiser, A. P. (2016). Intervention effects on spoken-language outcomes for children with autism: A systematic review and meta-analysis. Journal of Intellectual Disability Research, 60(5), 444–463. https://doi.org/10.1111/jir.12283
Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed.). Guilford Publications.
Ingersoll, B., & Gergans, S. (2007). The effect of a parent-implemented imitation intervention on spontaneous imitation skills in young children with autism. Research in Developmental Disabilities, 28(2), 163–175. https://doi.org/10.1016/j.ridd.2006.02.004
Johnson, M. H., Senju, A., & Tomalski, P. (2015). The two-process theory of face processing: Modifications based on two decades of data from infants and adults. Neuroscience & Biobehavioral Reviews, 50, 169–179. https://doi.org/10.1016/j.neubiorev.2014.10.009
Jones, W., & Klin, A. (2013). Attention to eyes is present but in decline in 2–6-month-old infants later diagnosed with autism. Nature, 504(7480), 427–431. https://doi.org/10.1038/nature12715
Kasari, C., Gulsrud, A., Paparella, T., Hellemann, G., & Berry, K. (2015). Randomized comparative efficacy study of parent-mediated interventions for toddlers with autism. Journal of Consulting and Clinical Psychology, 83(3), 554. https://doi.org/10.1037/a0039080
Koegel, R. L., Vernon, T. W., & Koegel, L. K. (2009). Improving social initiations in young children with autism using reinforcers with embedded social interactions. Journal of Autism and Developmental Disorders, 39(9), 1240–1251. https://doi.org/10.1007/s10803-009-0732-5
Landa, R. J. (2018). Efficacy of early interventions for infants and young children with, and at risk for, autism spectrum disorders. International Review of Psychiatry, 30(1), 25–39. https://doi.org/10.1080/09540261.2018.1432574
Lord, C., Luyster, R., Gotham, K., & Guthrie, W. (2012). Autism diagnostic observation schedule (2nd ed.). Western Psychological Services.
Maenner, M. J., Shaw, K. A., Bakian, A. V., Bilder, D. A., Durkin, M. S., Esler, A., Furnier, S. M., Hallas, L., Hall-Lande, J., Hudson, A., Hughes, M. M., Patrick, M., Pierce, K., Poynter, J. N., Salinas, A., Shenouda, J., Vehorn, A., Warren, Z., Constantino, J. N., et al. (2021). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2018. MMWR Surveillance Summaries, 70(11), 1–16.
Manly, C. A., & Wells, R. S. (2015). Reporting the use of multiple imputation for missing data in higher education research. Research in Higher Education, 56(4), 397–409. https://doi.org/10.1007/s11162-014-9344-9
Mullen, E. M. (1995). Mullen Scales of early learning. American Guidance Service.
Mundy, P. C. (2016). Autism and joint attention: Development, neuroscience, and clinical fundamentals. Guilford Publications.
Mundy, P., & Bullen, J. (2022). The bidirectional social-cognitive mechanisms of the social-attention symptoms of autism. Frontiers in Psychiatry. https://doi.org/10.3389/fpsyt.2021.752274
Nahmias, A. S., Pellecchia, M., Stahmer, A. C., & Mandell, D. S. (2019). Effectiveness of community-based early intervention for children with autism spectrum disorder: A meta-analysis. Journal of Child Psychology and Psychiatry, 60(11), 1200–1209. https://doi.org/10.1111/jcpp.13073
Ohashi, J. K., Mirenda, P., Marinova-Todd, S., Hambly, C., Fombonne, E., Szatmari, P., Bryson, S., Roberts, W., Smith, I., Vaillancourt, T., Volden, J., Waddell, C., Zwaigenbaum, L., Georgiades, S., Duku, E., Thompson, A., Pathways in ASD Study Team. (2012). Comparing early language development in monolingual-and bilingual-exposed young children with autism spectrum disorders. Research in Autism Spectrum Disorders, 6(2), 890–897. https://doi.org/10.1016/j.rasd.2011.12.002
Reichow, B. (2012). Overview of meta-analyses on early intensive behavioral intervention for young children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(4), 512–520. https://doi.org/10.1007/s10803-011-1218-9
Rollins, P. R., Campbell, M., Hoffman, R. T., & Self, K. A. (2016). A community-based early intervention program for toddlers with Autism Spectrum Disorders. Autism: The International Journal of Research and Practice, 20(2), 219–232. https://doi.org/10.1177/1362361315577217
Rollins, P. R., De Froy, A., Campbell, M., & Hoffman, R. T. (2021). Mutual gaze: An active ingredient for social development in toddlers with ASD: A randomized control trial. Journal of Autism and Developmental Disorders, 51(6), 1921–1938. https://doi.org/10.1007/s10803-020-04672-4
Rollins, P. R., John, S., Jones, A., & De Froy, A. (2019). Pathways Early ASD Intervention as a moderator of parenting stress on parenting behaviors: A randomized control trial. Journal of Autism and Developmental Disorders, 49(10), 4280–4293. https://doi.org/10.1007/s10803-019-04144-4
Rush, D. D., & Shelden, M. L. L. (2011). The early childhood coaching handbook. Brookes.
Sameroff, A. (2009). The transactional model. American Psychological Association. https://doi.org/10.1037/11877-001
Sandbank, M., Bottema-Beutel, K., Crowley, S., Cassidy, M., Dunham, K., Feldman, J. I., Crank, J., Albarran, S. A., Raj, S., Mahbub, P., & Woynaroski, T. G. (2020a). Project AIM: Autism intervention meta-analysis for studies of young children. Psychological Bulletin, 146(1), 1–29. https://doi.org/10.1037/bul0000215
Sandbank, M., Bottema-Beutel, K., Crowley, S., Cassidy, M., Feldman, J. I., Canihuante, M., & Woynaroski, T. (2020b). Intervention effects on language in children with autism: A project AIM meta-analysis. Journal of Speech, Language, and Hearing Research, 63(5), 1537–1560. https://doi.org/10.1044/2020_JSLHR-19-00167
Schertz, H. H., Baker, C., Hurwitz, S., & Benner, L. (2011). Principles of early intervention reflected in toddler research in autism spectrum disorders. Topics in Early Childhood Special Education, 31(1), 4–21. https://doi.org/10.1177/0271121410382460
Schertz, H. H., Reichow, B., Tan, P., Vaiouli, P., & Yildirim, E. (2012). Interventions for toddlers with autism spectrum disorders: An evaluation of research evidence. Journal of Early Intervention, 34(3), 166–189. https://doi.org/10.1177/1053815112470721
Schreibman, L., Dawson, G., Stahmer, A. C., Landa, R., Rogers, S. J., McGee, G. G., Kasari, C., Ingersoll, B., Kaiser, A. P., Bruinsma, Y., McNerney, E., Wetherby, A., & Halladay, A. (2015). Naturalistic developmental behavioral interventions: Empirically validated treatments for autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(8), 2411–2428. https://doi.org/10.1007/s10803-015-2407-8
Senju, A., & Johnson, M. H. (2009). Atypical eye contact in autism: Models, mechanisms and development. Neuroscience & Biobehavioral Reviews, 33(8), 1204–1214. https://doi.org/10.1016/j.neubiorev.2009.06.001
Shire, S. Y., Shih, W., Gelfand, C., & Kasari, C. (2016). Preschool deployment of evidence-based social communication intervention: JASPER in the classroom. Journal of Autism and Developmental Disorders, 46(6), 2211–2223. https://doi.org/10.1007/s10803-016-2752-2
Siller, M., Hutman, T., & Sigman, M. (2013). A parent-mediated intervention to increase responsive parental behaviors and child communication in children with ASD: A randomized clinical trial. Journal of Autism and Developmental Disorders, 43(3), 540–555. https://doi.org/10.1007/s10803-012-1584-y
Snow, C. E. (1999). Social perspectives on the emergence of language. In B. MacWhinney (Ed.), The emergence of language (pp. 257–276). Erlbaum.
Sparrow, S. S., Cicchetti, D. V., & Balla, D. A. (2005). Vineland Adaptive Behavior Scales (2nd ed.). NCS Pearson.
Stronach, S. T., & Wetherby, A. M. (2017). Observed and parent-report measures of social communication in toddlers with and without autism spectrum disorder across race/ethnicity. American Journal of Speech-Language Pathology, 26(2), 355–368. https://doi.org/10.1044/2016_AJSLP-15-0089
Tomasello, M., Carpenter, M., Call, J., Behne, T., & Moll, H. (2005). Understanding and sharing intentions: The origins of cultural cognition. Behavioral and Brain Sciences, 28(5), 675–691. https://doi.org/10.1017/S0140525X05000129
United States Census Bureau. (n.d.). Quick facts. Dallas, TX.
van Ginkel, J. R. (2019). Significance tests and estimates for R 2 for multiple regression in multiply imputed datasets: A cautionary note on earlier findings, and alternative solutions. Multivariate Behavioral Research, 54(4), 514–529. https://doi.org/10.1080/00273171.2018.1540967
Vygotsky, L. S. (1978). Mind in society: The development of higher psychological processes. Harvard University Press.
Wallace, K. S., & Rogers, S. J. (2010). Intervening in infancy: Implications for autism spectrum disorders. Journal of Child Psychology and Psychiatry, 51(12), 1300–1320. https://doi.org/10.1111/j.1469-7610.2010.02308.x
Wetherby, A., & Prizant, B. (2002). Communication and Symbolic Behavior Scales—Developmental profile (1st ed.). Paul-H-Brookes.
Wetherby, A. M., Woods, J., Guthrie, W., Delehanty, A., Brown, J. A., Morgan, L., Holland, R. D., Schatschneider, C., & Lord, C. (2018). Changing developmental trajectories of toddlers with autism spectrum disorder: Strategies for bridging research to community practice. Journal of Speech, Language, and Hearing Research, 61(11), 2615–2628. https://doi.org/10.1044/2018_JSLHR-L-RSAUT-18-0028
What Works Clearinghouse. (2020). What Works Clearinghouse Standards Handbook, Version 4.1. U.S. Department of Education, Institute of Education Sciences, National Center for Education Evaluation and Regional Assistance. Retrieved from https://ies.ed.gov/ncee/wwc/Docs/referenceresources/WWC-Standards-Handbook-v4-1-508.pdf
Yoder, P. J., Bottema-Beutel, K., Woynaroski, T., Chandrasekhar, R., & Sandbank, M. (2013). Social communication intervention effects vary by dependent variable type in preschoolers with autism spectrum disorders. Evidence-Based Communication Assessment and Intervention, 7(4), 150–174. https://doi.org/10.1080/17489539.2014.917780
Yoder, P. J., & Crandall, M. (2019). Rationale for blindness to treatment assignment in between-group experiments testing generalized communication and language. Evidence-Based Communication Assessment and Intervention, 13(4), 225–229. https://doi.org/10.1044/2019_JSLHR-L-18-0081
Zwaigenbaum, L., Bauman, M. L., Stone, W. L., Yirmiya, N., Estes, A., Hansen, R. L., McPartland, J. C., Natowicz, M. R., Choueiri, R., Fein, D., Kasari, C., Pierce, K., Buie, T., Carter, A., Davis, P. A., Granpeeshe, D., Mailloux, Z., Newschaffer, C., Robins, D., et al. (2015). Early identification of autism spectrum disorder: Recommendations for practice and research. Pediatrics, 136(Supplement 1), S10–S40. https://doi.org/10.1542/peds.2014-3667C
Acknowledgments
This research was supported by a Grant from the Texas Higher Education Coordinating Board’s Autism Grants Program. The opinions and conclusions expressed are those of the authors and do not necessarily represent the opinions or policy of the THECB. This project has received IRB approval (IRB 18-149) from the University of Texas at Dallas. The authors would like to thank the children and families who participated in this study, the clinical researchers who provided intervention.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Rollins has received research grants from the Texas Higher Education Coordinating Board’s (THECB) Autism Grant Program and has received speaker honorariums for several speaking engagements. De Froy’s research assistantship is supported by THECB Autism Grant (Rollins, PI).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rollins, P.R., De Froy, A.M. Reexamining Pathways Early Autism Intervention in Children Before and After the Third Birthday: A Randomized Control Trial. J Autism Dev Disord 53, 1189–1201 (2023). https://doi.org/10.1007/s10803-022-05599-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-022-05599-8