Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Infectious disease
Covid-19
COVID-19 is probably more deadly to men than women, but scientists still aren’t sure why
Most available data suggest men may be more likely to die from coronavirus infections, but the reason why could be complicated
by Leigh Krietsch Boerner
July 27, 2020
| A version of this story appeared in
Volume 98, Issue 29

Throughout the COVID-19 pandemic, news stories have reported a troublesome trend: men seem to be more likely to get sick and die from the disease than women.
However, scientists studying available data on who is getting infected by SARS-CoV-2 admit the picture is far from clear. Holes in the data, such as missing demographic information and lack of widespread testing in some populations, make it difficult to come to a conclusion about men and women’s relative risks. But overall, it does seem like men are more likely to die from COVID-19 than women.
Why such a difference could exist is also tricky to explain. Some scientists point to behavioral and social differences between men and women, such as smoking or regularly seeing a doctor, that could affect disease severity. Meanwhile, biological differences in men and women’s immune systems could explain men’s higher COVID-19 risk.
As the pandemic thunders on and scientists accumulate more information, they’re analyzing it to understand possible sources for this risk difference between men and women. “It may be related to immunity, it may be related to sex hormones, it may be related to behaviors, it may be related to men having more health problems like diabetes and cardiovascular disease,” says Erin Michos, a cardiologist at Johns Hopkins University. “I think it’s going to be a lot of things.”
Show me the data
Sources: World Health Organization, Global Health 5050 Note: Data pulled 7/13/20

Sources: World Health Organization, Global Health 5050 Note: Data pulled 7/13/20

Trying to tease out why men and women experience different health outcomes—not just for COVID-19—is complicated by the fact that defining sex is not easy. “No simple definition of biological sex works for everyone, because there are people with mixtures of male and female characteristics, who are not easily classified as male or female by any simple rule,” says Arthur Arnold, a biologist and physiologist at the University of California, Los Angeles. These distinctions also become more complicated when a scientist takes gender into account, which involves social and behavioral attributes and not biological ones.
When scientists run studies to understand health differences, they generally do not run tests to determine a person’s sex chromosomes, Arnold says. “In many cases, men and women self-report or check a box on a form,” he says.
When reporting deaths it’s sometimes unclear how coroners and medical professionals assign sex to the deceased, and the procedures can vary from place to place, says Heather Shattuck-Heidorn, who studies sex and gender in public health at the University of Southern Maine, and is an assistant director at Harvard University’s GenderSci Lab. “It is likely that some trans and probably most nonbinary people are being misreported,” she says. Coroners and medical professionals may use the sex that’s listed on medical forms or on a person’s birth certificate. In many US states, the sex on a person’s birth certificate can be legally changed, and some states offer nonbinary sex options. However, those states are the minority.
In this article, we’re using the terms women and men to describe people who identify as such.
In addition to those general complexities about defining sex, researchers have also struggled to get enough data to try to identify a COVID-19 risk difference between men and women. Global Health 5050, an independent research group, has been collecting data broken down by sex on COVID-19 since March. The GenderSci Lab COVID Project at Harvard has also been tracking the data back to April. Both groups say that separate COVID-19 data for men and women have been hard to come by.
For example, while the US Centers for Disease Control and Prevention asks that states report age, sex, and race of COVID-19 patients, some states don’t, Shattuck-Heidorn says. Each state runs its own public health system and the way they collect data is not standardized.
In the US, the data also don’t give the full picture of who has been infected because testing has been limited, says Nir Menachemi, who studies health policy and management at the Fairbanks School of Public Health at IUPUI. Up until recently, in many places in the US, only people at the highest risk of serious illness and those with the most severe COVID-19 symptoms got tested. That left out people who were infected but asymptomatic and people who were not deemed sick enough to get a test.
Deaths from COVID-19 are also likely underreported, Shattuck-Heidorn says. Some places in the US still aren’t reporting people who died at home or in nursing homes or people who died without an official COVID-19 diagnosis. Not counting some of those deaths could skew sex differences in the data, she says. For example, “there are many more women in nursing homes than men. So if women are being systematically underreported because [they died at] nursing homes, that would inflate the male death rate.”
Global Health 5050 reports that in countries with available data, there is no clear picture of whether women or men are more likely to be diagnosed with COVID-19. But the organization points out that in all countries, more men are dying from the disease than women. The GenderSci Lab COVID Project, which tracks just US data, reports a similar sex difference for COVID-19 deaths. But it does find a large variation in the difference from state to state. In a recently published study, another group of researchers looked at data from 17 million patients in the UK and found that, overall, men were more likely to die from COVID-19 than women, and this difference increased with age (Nature, 2020. DOI: 10.1038/s41586-020-2521-4).
Deciphering the difference
The data pointing to a higher COVID-19 death rate for men don’t surprise Andrew Noymer, who studies population health and disease prevention at the University of California, Irvine. “Men are more susceptible to just about every infection, which is one of the reasons they live less long,” he says. “COVID-19 is adhering to expectations on the sex differences. I realize that’s not a sexy quote for your readers. But it’s the truth.”
There were sex differences in both who got sick and who died during the other two major coronavirus outbreaks, the 2002–3 severe acute respiratory syndrome (SARS) outbreak and the 2015 Middle East respiratory syndrome (MERS) outbreak, Shattuck-Heidorn says. With MERS, men had higher rates of infection and death, while men had higher death rates with SARS. “The same is true for more historical data, such as the 1918 influenza pandemic,” she says.

Death rates from COVID-19 are definitely related to underlying health problems such as heart disease or diabetes, which kill men more often than women, Noymer says. When researchers analyzed data from the SARS and MERS outbreaks, the differences in infection and death between men and women could be explained by differences in these underlying health issues, Shattuck-Heidorn says.
There are also some social and behavioral differences between men and women that could influence overall health and COVID-19 risk. For example, men smoke and drink more than women, although how much more varies greatly across the globe. Men are also less likely to wash their hands. It’s also a matter of exposure, says immunologist Veena Taneja of the Mayo Clinic. In some parts of the world, men are more likely to be out in the workforce, she says, which means that men are more likely to be exposed to the virus.
The biological factor
In terms of the role biology plays in these risk differences between men and women, experts point to the immune system as the key player. Women generally have more robust immune systems than men do, Taneja says.
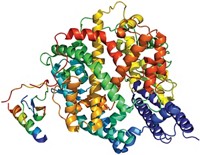
Many genes involved in how our immune systems respond to pathogens live on our X chromosomes. In most cases, men’s sex chromosomes are XY, so they have only one copy of these X chromosome genes. Women typically are XX, giving them two copies. Scientists have observed that these genes can be active on both chromosomes at the same time, Taneja says. Having both genes active allows immune cells in women to make more of the antibodies that help neutralize threats.
In addition, the immune response to a virus or bacteria differs some between the sexes. When our bodies encounter an invading pathogen, two types of white blood cells, called lymphocytes, attack it. These lymphocytes—B cells and T cells—each recognize pathogens in different ways. T cells come in two types: CD8+ T cells, which destroy infected cells, and CD4+ T cells, which direct this attack. B cells don’t do any killing, but they make antibodies that target pathogens for an attack, and they clear infected cells out of the system after T cells launch their assault.
Men and women tend to have the same amount of T cells, but women generally have more B cells than men do, Taneja says. Having more B cells means women’s immune systems are better equipped to recognize invading threats for T cells to target.
Women and men’s CD4+ T cells also produce different kinds of immune signaling molecules called cytokines. Men produce more of a kind that promotes inflammation, while women make more that help clear pathogens. In some patients with severe forms of COVID-19, their immune systems overproduce inflammatory cytokines, leading to harmful swelling, pain, organ damage, and in some cases death. Once this so-called cytokine storm gets rolling, T cells just keep churning out the molecules. “The T cells are activated so much that the body is unable to control them,” Taneja says. B cells can help rein in this out-of-control inflammation, shielding the body from the raging storm, which may explain why women may not develop more severe forms of COVID-19.
Finally, sex hormones play a role in our immune responses. Women tend to have higher levels of estrogen than men do, and that hormone can upregulate genes involved in B cell activation and survival, rendering them more resistant to cell death. This estrogen-powered protection of B cells reinforces the immune-boosting benefits women get from the immune cells. Cell receptors that bind estrogen are present in many tissues where SARS-CoV-2 is thought to attack, Taneja says, such as in the lungs and intestines.
However, much of this estrogen-related immune protection disappears during menopause when women’s estrogen levels drop suddenly, Taneja says. But, this drop in immune protection at menopause doesn’t seem to affect COVID-19 risk, Michos says. “If it were all related to hormones, older women would do just as badly as older men.” Some scientists see sex differences for COVID-19 across all age groups, she says, not just younger ones.
In general, scientists seem to agree on one thing: they don’t know what’s causing the sex difference for COVID-19 deaths. There’s good evidence that this difference is probably not due to just biology, Shattuck-Heidorn says. “I think we have this pretty myopic focus on how innate sex is probably driving these differences,” she says. “Given that the data is a mess, it’s too early to really say,” but researchers need to frame the issue in a variety of ways.
Scientists, Shattuck-Heidorn says, need to run studies that take into account a range of variables like underlying health conditions, age, smoking, and exposure risks. Then the researchers need to analyze how these different variables interact with each other, potentially allowing researchers to understand whether these factors can explain differences in infection and death rates instead of sex. And if sex does seem to play a significant role, she says, studies will need to be done to see exactly what that role is.
Some scientists are trying to do such studies, and others are calling for sex and gender factors to be included in COVID-19 research. But for past coronavirus outbreaks, the key to solving this issue was collecting enough data to understand the role different risk factors played. At this point in the COVID-19 pandemic, scientists just don’t have enough data yet.


Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter